More Information
Submitted: March 04, 2025 | Approved: March 12, 2025 | Published: March 14, 2025
How to cite this article: Mercês Silva AD. Impact of the MELD Scale on Hospital Admissions for Hepatocarcinoma (2000 to 2018), Brazil. J Community Med Health Solut. 2025; 6(1): 027-033. Available from:
https://dx.doi.org/10.29328/journal.jcmhs.1001054
.
DOI: 10.29328/journal.jcmhs.1001054
Copyright license: © 2025 Mercês Silva AD. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: MELD; Hospitalizations; Hepatocarcinoma
Impact of the MELD Scale on Hospital Admissions for Hepatocarcinoma (2000 to 2018), Brazil
Alexandro das Mercês Silva*
University of São Paulo, Brazil
*Address for Correspondence: Alexandro das Mercês Silva, Data Science Specialist, Specialist in Procurement, Donation, and Transplantation of Organs and Tissues, University of São Paulo, Brazil, Email: [email protected]
Background: The health professional appears to be concerned given the number of questions surrounding the patient’s post-transplant survival, patient selection method, and the continuous search for scores that reflect their reality and reconcile the results they desire with the patient’s expectations. It is from these considerations that the present work was born with the purpose of understanding the reality of patients hospitalized for hepatocellular carcinoma and what adherence to the Model For End-Stage Liver Disease (MELD) criteria meant in Brazil.
Methods: This study is a discrete, univariate time series on emergency hospitalizations that occurred between 2000 and 2018, in the city of São Paulo, Brazil. Python version 3.11 was the software used for statistical treatment and analysis of the time series.
Results: There were 6887 hospitalizations for malignant neoplasm of liver and intrahepatic bile ducts, in the period 2000-2006, of which 2898 were elective and 3915 (56.85%) were urgent in the period. There was an increase of 63.97% in the number of emergency hospitalizations in relation to the period 2000-2006 and 2007-2013. To highlight, in 2013 there were 1270 emergency admissions, which represented an increase of 109.22% in relation to the number of emergency admissions in 2006. The contingency correlation analysis demonstrated a significant association between the variables in which the chi-square value was 82.18, the p-value was 1.24 x 10-19, and the critical value was 3.84 with one degree of freedom. There was a 123.65% increase in the number of hospitalizations for chronic hepatitis, not elsewhere classified, between the periods 2000-2006 and 2007-2013. The chi-square value of the contingency association was 221.22, with a p-value of 4.90 x 10-50, a critical value of 9.488, with a significance level of 5% and one degree of freedom. The study showed an increase in hospitalizations of 21.88% for alcoholic liver disease between the periods 2000-2006 and 2007-2013. In the period 2000-2006, there were 21330 hospitalizations, 19224 of which were urgent (90.13%). In the period 2007-2013, there were 25997 hospitalizations, of which 22,802 (87.71%) occurred urgently. The chi-square value was 68.95, the p-value was 1 x 10-16, and the critical value was 3.84, with one degree of freedom.
Conclusion: The MELD score, as it is sensitive to the patient’s severity, selects those who are at an advanced stage of the disease for liver transplantation. In this scenario, patients do not necessarily have access to outpatient services and begin to attend them regularly when MELD identifies the advanced stage of the disease, opening a gap between prevention, treatment, and rehabilitation.
The adoption of the Model For End-Stage Liver Disease (MELD) criteria will complete 20 years in Brazil in 2026. At the beginning of liver transplant programs, deceased donors in the State of São Paulo were allocated to different teams, on a daily scale, according to the number of candidates at each institution. In 1997, the legislation on organ transplants was regulated, and the Single List of Recipients was adopted, and coordinated by the State Department of Health, which considered the chronological order for carrying out the transplant [1,2].
In 2006, the criteria for distributing livers from deceased donors for transplantation was changed, with the severity criterion (MELD) being implemented. To be included on the waiting list, the patient undergoes evaluation by a transplant team, which places them on the waiting list. As soon as the patient is registered, they receive a registration number through which they can obtain information about their status on the waiting list, which can be: Active; Semi-active; or Removed. The distribution of the organ is made to registered patients and only those with Active status participate [3-5].
The MELD score (Model for End-Stage Liver Disease), a model initially created to estimate three-month survival in patients undergoing transjugular intrahepatic portosystemic venous shunt, has as variables the serum levels of creatinine, total bilirubin, and the international standardized ratio for prothrombin time (INR) being calculated by the formula:
MELD = 10*((0.957*Ln[Creatinine mg/dl] + (0.378 * Ln [Bilirubin mg/dl] + (1.12 * Ln[INR] + 6.43 * 10
In 2006, the MELD score was adopted in Brazil and the recommended exams must be renewed periodically [6-10].
MELD from 11 to 18 – valid for three months, exam taken in the last 14 days;
MELD from 19 to 25 – valid for one month, exam taken in the last 7 days;
MELD greater than 25 – valid for seven days, test taken in the last 48 hours.
The literature highlights the concern of health professionals given the number of questions surrounding post-transplant survival, patient selection, and the continuous search for scores that reflect their understanding of the professional reality and reconcile the results they desire with the expectations of patients [8,10-15].
It was from these considerations that the present work was born with the objective of analyzing and understanding, through a temporal study, the meaning, and impact of adherence to the MELD criteria on the process of deceased donor liver transplantation in the state of São Paulo, Brazil.
This study is a discrete, univariate time series on emergency hospitalizations that occurred between 2000 and 2018, in the city of São Paulo, Brazil. Python version 3.11 was the software used for statistical treatment and analysis of the time series.
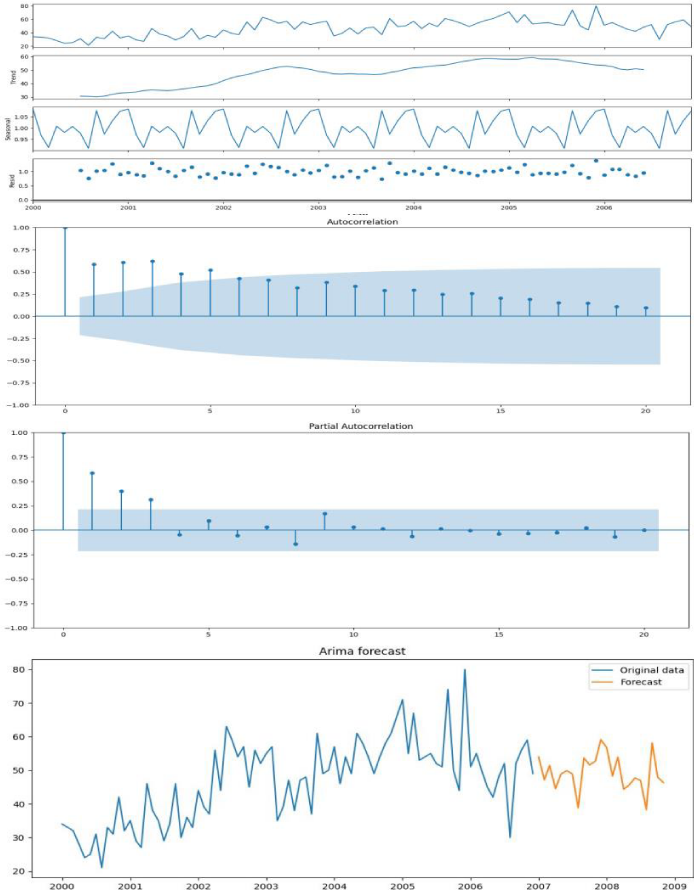
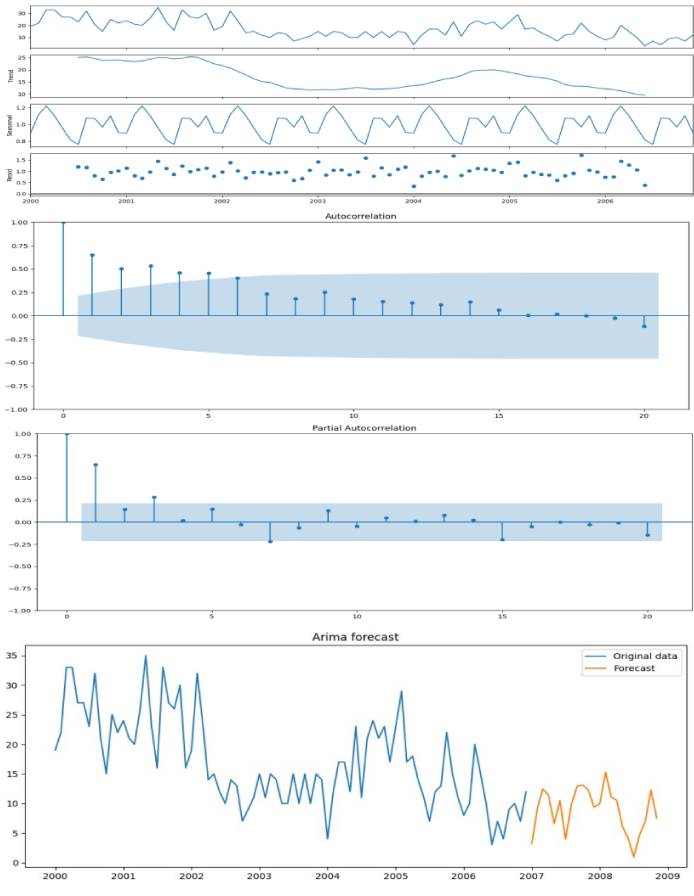
To construct the forecast or projection model, data were aggregated into two periods: The period before the adoption of MELD (2000-2006) and the MELD period (2007-2013). For the Arima Seasonal prediction model, the period 2000-2006 was used and the projection results for the next 24 months were compared, comprising the years 2007 and 2008.
The data were subjected to multiplicative decomposition, stationarity test using the Dickey-Fuller test, correlogram of autocorrelation and partial autocorrelation functions, exponential smoothing, and finally the Arima Seasonal method was used to carry out the forecast, projection of hospitalizations 24 months after the adoption of MELD.
Still in relation to the two periods (2000-2006 and 2007-2013), a contingency analysis was carried out using the frequency of emergency and non-urgent hospitalizations. The conclusion of the analysis was supported by the calculation of the chi-square value, p-value, critical value, and degree of freedom.
The extracted data corresponds to the Hospital Admission Authorization stored in the Hospital Information System, which records all hospital admissions that were financed by the Brazilian National Health System. The Hospital Admission Authorization is only generated when the patient is admitted and provides information about the main reason for hospitalization, location, period of hospitalization, age, sex, procedures performed, etc. These data are made available for consultation in the DataSUS Health Information System-Tabnet.
To describe the distribution of hospitalizations for hepatocellular carcinoma, data were collected according to the 3-digit ICD-10 diagnostic groups that characterize hepatocellular carcinoma: acute hepatitis B, other acute viral hepatitis, chronic viral hepatitis, malignant neoplasm of liver and intrahepatic bile ducts, alcoholic liver disease, hepatic failure- not elsewhere classified, chronic hepatitis- not elsewhere classified, fibrosis and cirrhosis of the liver, and other diseases of the liver.
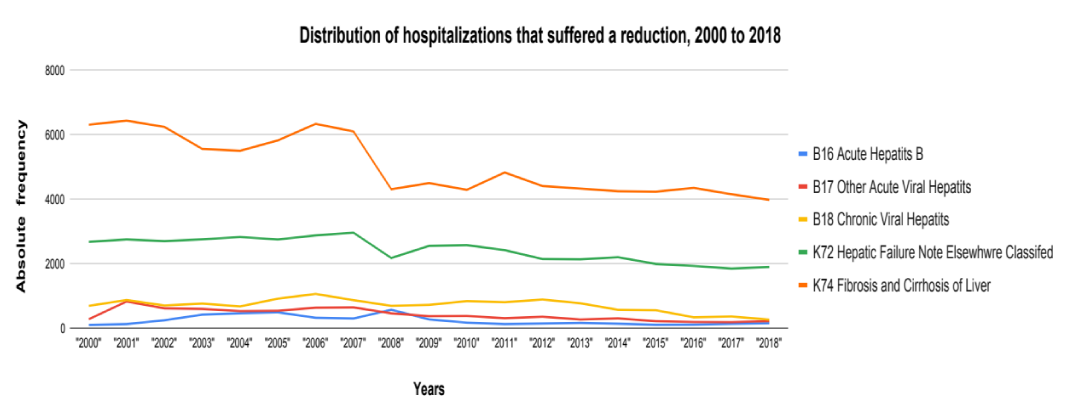
The adoption of the MELD criteria represented a reduction in hospitalizations of patients diagnosed with B16 - acute hepatitis B, B17 - other acute viral hepatitis, B18 - chronic viral hepatitis, K72 - liver failure not classified elsewhere, and K74 - liver fibrosis and cirrhosis.
However, patients diagnosed with C22 - malignant neoplasm of the liver and intrahepatic bile ducts, K70 - alcoholic liver disease, K73 - chronic hepatitis not classified elsewhere, and K76 - other liver diseases showed an increase in the number of hospitalizations.
The reduction in hospitalizations due to K72 - liver failure not classified elsewhere was accompanied by an increase in the number of liver transplants, a result also presented by K74 - liver fibrosis and cirrhosis. The diagnosis of K70 - alcoholic liver disease also showed an increase in the number of transplants, but this diagnosis was accompanied by an increase in the number of hospitalizations (Figure 1).
Figure 1: Distribution of hospitalizations that suffered reduction, 2000 to 2018. Source: SESSP/SIH-SUS - Hospital Information System.
However, patients diagnosed with alcoholic liver disease, malignant neoplasm of the liver and intrahepatic bile ducts, other liver diseases, and chronic hepatitis not classified elsewhere showed an increase in the number of hospitalizations, with these diagnoses being subjected to time series and correlation studies.
ICD 10: C22 - Malignant neoplasm of liver and intrahepatic bile ducts
Malignant neoplasm of the liver and intrahepatic bile ducts fall into the subgroup formed by the diagnoses hepatic cell carcinoma, intrahepatic bile duct carcinoma, hepatoblastoma, angiosarcoma of the liver, other sarcomas of the liver, other specified carcinomas of the liver, malignant neoplasm of the liver, and unspecified.
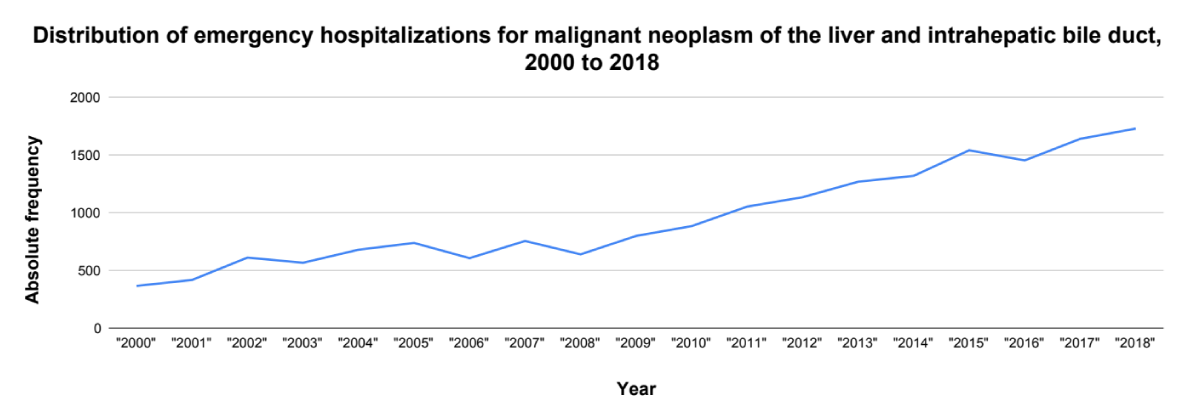
Admissions of adults remain regular, suggesting readmissions of the same group of patients and it is likely that this period is a period of tumor staging, making the incidence of signs and symptoms present from middle age or from the age of 60 onwards resulting in an increase in hospitalizations (Figure 2) [16-19].
Figure 2: Distribution of emergency hospitalizations for malignant of the liver and intrahepatic bile duct, 2000 to 2018. Source: SESSP/SIH-SUS - Hospital Information System.
These results are in line with what the literature states about some diagnoses that constitute the ICD C22 subgroup, such as carcinoma of the intrahepatic bile ducts, which progresses without signs and symptoms, and only manifests at a more advanced stage of the disease when the patient is middle-aged (45 to 59) or elderly (60 years or more) [20-22].
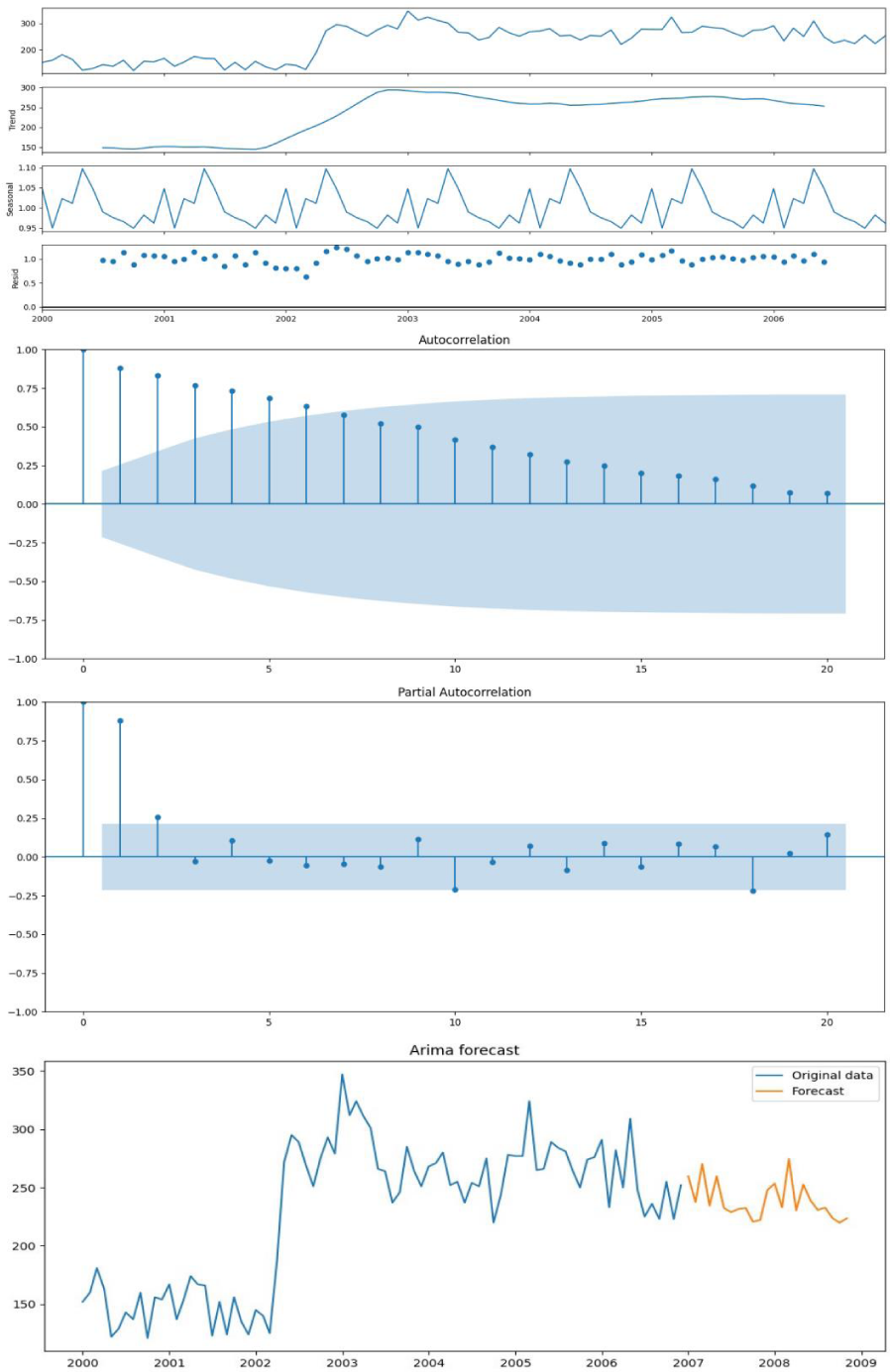
The Arima model chosen for the study presented AIC: 600.01, BIC: 609.72, HQIC: 603.93, and Ljung-Box: 0. The value of the partial autocorrelation function exceeds the significance threshold of 5% in lags 1, 2 and 3. In relation to the accuracy of the model, the Mean Square Error (MSE) is 75.45.
According to the series, emergency hospitalizations showed significant growth in 2001, reaching a peak in 2005, and showing a downward trend from 2006 onwards. The forecast, according to the Arima model, is for a lower number of hospitalizations than in 2006, however, the data observed in 2007 indicate an increase in hospitalizations, and from 2008 onwards, hospitalizations assume linear growth (Figure 3).
Figure 3: Seasonal Arima Model for Emergency Admissions for Malignant Neoplasms of the Liver and Intrahepatic Biliary Tract, 2000 to 2018.
There were 6887 hospitalizations in the period 2000-2006, of which 2898 were elective and 3915 (56.85%) were urgent in the period. There was an increase of 63.97% in the number of emergency hospitalizations in relation to the period 2000-2006 and 2007-2013. To highlight, in 2013 there were 1270 emergency admissions, which represented an increase of 109.22% in relation to the number of emergency admissions in 2006.
The contingency correlation analysis demonstrated a significant association between the variables in which the chi-square value was 82.18, the p-value was 1.24 x 10-19, and the critical value was 3.84 with one degree of freedom.
While adults showed constant values in the number of hospitalizations between the periods 2000-2006 and 2007-2013, the middle-aged age group registered an increase of 88.51% between the periods 2000-2006 (1097 emergency admissions) and 2007-2013 (2068 emergency admissions).
ICD 10: K70 - Alcoholic liver disease
Alcoholic liver disease is made up of the following diagnostic subgroups: alcoholic fatty liver, alcoholic hepatitis, fibrosis and alcoholic sclerosis of the liver, alcoholic liver cirrhosis, alcoholic liver failure, and alcoholic liver disease- not otherwise specified.
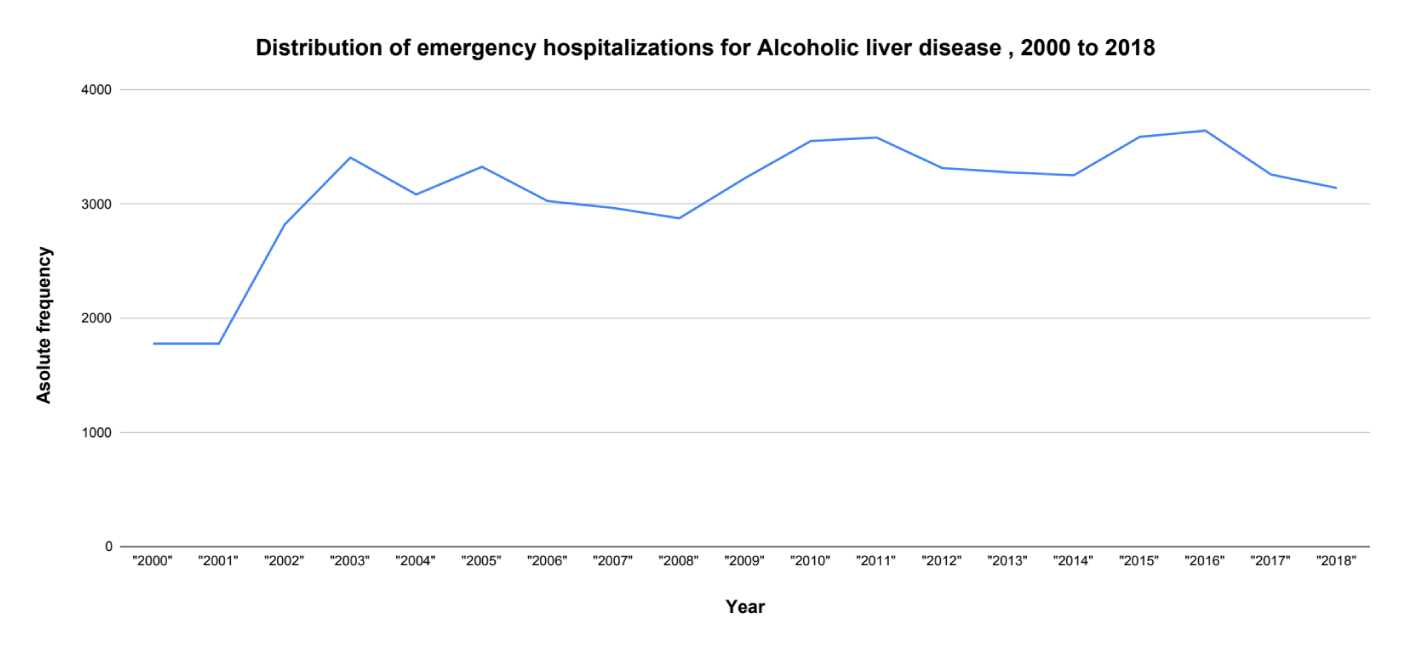
Steatosis is the first stage and can be reversed, followed by fibrosis and cirrhosis. Studies show that cirrhosis is more prevalent in middle-aged people (45 to 59 years old). During adulthood (20 to 44 years) the disease progresses and in middle age, the diagnosis of cirrhosis is made. The MELD score, being sensitive to the patient’s severity, selects patients at an advanced stage of the disease, leaving adult patients (20 to 44 years old) without screening, prevention, and outpatient care measures [23-26].
Therefore, interventions in middle-aged patients are not felt through a reduction in hospitalizations because adult patients progress to a more severe stage of the disease, increasing the number of hospitalized patients (Figure 4) when they enter middle age. Adult patients do not necessarily have access to outpatient or prevention services, having access to assistance and attending the outpatient clinic regularly when the MELD identifies the advanced stage of the disease [27-34].
Figure 4: Distribution of emergency hospitalizations for Alcoholic liver disease, 2000 to 2018. Source: SESSP/SIH-SUS - Hospital Information System.
The Arima Model (2,1,1) presented AIC: 793.23, BIC: 802.12, and HQIC: 797.12. The residues appear as white noise given that the LJung-Box value: 0. In relation to the accuracy of the model, the Mean Square Error (MSE) is 914.48. It is worth mentioning the 136% growth in the number of hospitalizations between the months of March 2002 and June 2002. There are approximately two years (January 2000 to February 2002) in which the average number of hospitalizations is 147.73 hospitalizations with a variance of 13183.3 and a standard deviation of 114.81. Between March 2002 and June 2002, the average increased to 220 hospitalizations, a variance of 6126, and a standard deviation of 78.27 (Figure 5).
Figure 5: Seasonal Arima Model for Emergency Admissions for Alcoholic Liver Disease, 2000 to 2018.
The study showed an increase in hospitalizations of 21.88% between the periods 2000-2006 and 2007-2013. In the period 2000-2006, there were 21330 hospitalizations, 19224 of which were urgent (90.13%). In the period 2007-2013, there were 25997 hospitalizations, of which 22,802 (87.71%) occurred urgently. The chi-square value was 68.95, the p-value was 1 x 10-16, and the critical value was 3.84, with one degree of freedom.
ICD 10: K73 - Chronic hepatitis, not elsewhere classified
The K73 grouping - chronic hepatitis not elsewhere classified (NCOP) is made up of diagnostic subgroups: K73.0 - chronic hepatitis, not elsewhere classified; K73.1 - chronic lobular hepatitis not elsewhere classified; K73.2 - chronic active hepatitis, not classified elsewhere; K73.8 - other chronic hepatitis not classified elsewhere, and K73.9 - chronic hepatitis, not otherwise specified.
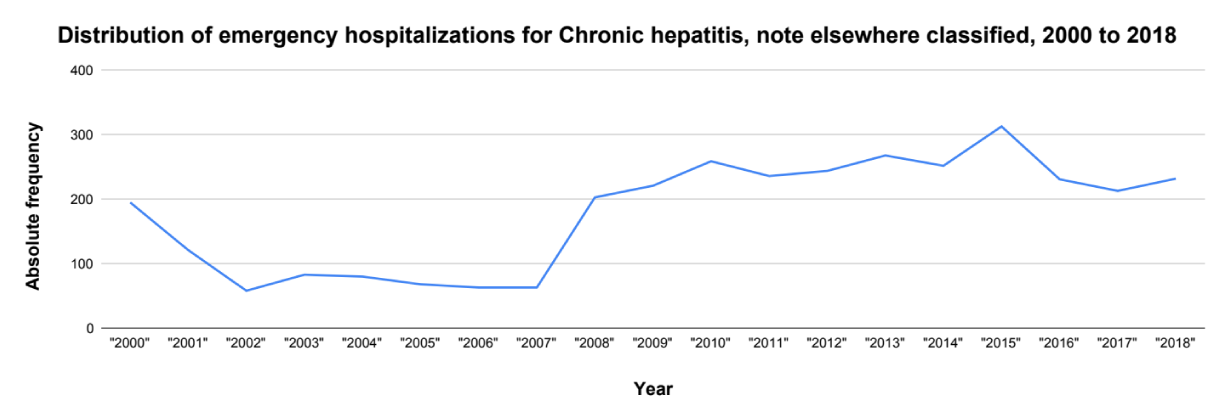
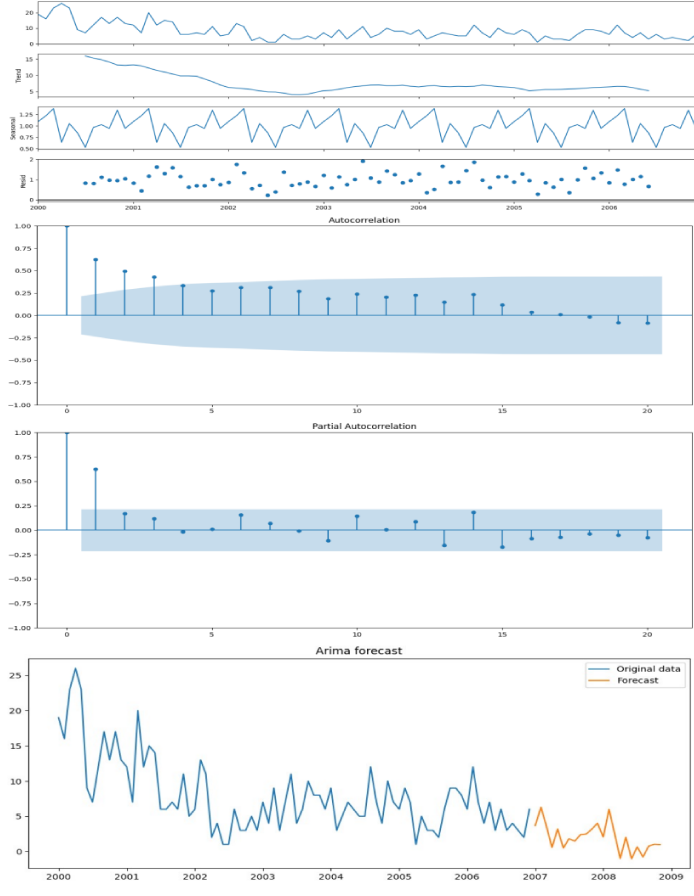
The period 2000-2006 recorded 1236 hospitalizations, of which 668 (54.4%) occurred urgently, while 2007-2013 presented 1887 hospitalizations, corresponding to 1494 hospitalizations or 79.1% of this total (Figure 6).
Figure 6: Distribution of emergency hospitalizations for chronic hepatitis, not elsewhere classified, 2000 to 2018. Source: SESSP/SIH-SUS - Hospital Information System.
The chosen Arima Model presented AIC: 463.82, BIC: 473.50, HQIC: 467.71, and LJung-Box: 0.07. Regarding the accuracy of the model, the Mean Square Error (MSE) is 7.68. According to the series, there is a decline in hospitalizations reaching the lowest value in 2003 and according to the graph the tendency would be to maintain hospitalization values at this level, however, the data observed show a significant increase in emergency hospitalizations in 2007 (Figure 7).
Figure 7: Seasonal Arima Model for Emergency Admissions for Chronic Hepatitis, not elsewhere classified, 2000 to 2018.
There was a 123.65% increase in the number of hospitalizations between the periods 2000-2006 and 2007-2013. The chi-square value of the contingency association was 221.22, with a p-value of 4.90 x 10-50, a critical value of 9.488, with a significance level of 5% and one degree of freedom.
ICD 10: K76 - Other diseases of liver
ICD 10 K76 is made up of the following diagnostic groups: fatty degeneration of the liver not classified elsewhere, chronic passive liver congestion, central hemorrhagic necrosis of the liver, liver infarction, peliosis hepatis, veno-occlusive liver disease, portal hypertension, hepatorenal syndrome, other specific liver diseases, and liver disease- not otherwise specified [35-39].
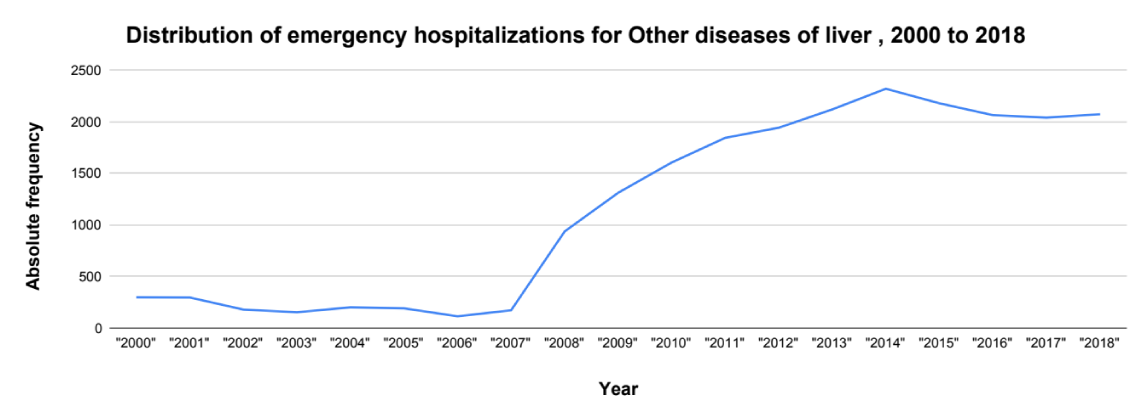
There was a significant increase in the number of hospitalizations between the periods 2000-2006 and 2007-2013. While in the period 2000-2006, 2769 hospitalizations were recorded, of which 1439 (51.96%) were urgent, in the period 2007-2013, 12110 hospitalizations were recorded, 9943 (82%) of which were urgent. The chi-square of the association was 1139, with a p - value of 1.1 x 10-249, a critical value of 9.488, with a significance level of 5% and one degree of freedom (Figure 8).
Figure 8: Distribution of emergency hospitalizations for other diseases of the liver, 2000 to 2018. Source: SESSP/SIH-SUS - Hospital Information System
The chosen Arima Model presented AIC: 525.21, BIC: 534.89, HQIC: 529.10, and LJung-Box: 0.01. Regarding the accuracy of the model, the Mean Square Error (MSE) is 30.77. According to the series, there is a decline in hospitalizations reaching the lowest value in 2003 and according to the graph the tendency would be to maintain hospitalization values at this level, however, the data observed show a significant increase in emergency hospitalizations in 2007 (Figure 9).
Figure 9: Seasonal Arima Model for Emergency Admissions for Other diseases of the liver, 2000 to 2018.
All age groups showed an increase in the number of hospitalizations. Highlighting emergency admissions, the group of children under one year of age in the period 2000-2006 recorded 34 admissions and in the period 2007-2013 there were 125 emergency admissions, an increase of 267.65%.
Children aged 1 to 9 years recorded 70 hospitalizations in the period 2000-2006 and 219 emergency hospitalizations in the period 2007-2013. Adolescents showed a 356% increase in the number of hospitalizations, registering 60 hospitalizations in the period 2000-2006 and 274 hospitalizations in the period 2007-2013.
423 adults were hospitalized in the period 2000-2006 and 2213 in the period 2007-2013, an increase of 423%. The middle-aged group recorded 467 emergency hospitalizations in the period 2000-2006 and 3530 hospitalizations in the period 2007-2013, an increase of 655%. Elderly people registered 385 emergency hospitalizations in the period 2000-2013 and 9943 in the period 2007-2013, an increase of 830%.
The MELD score, as it is sensitive to the patient’s severity, selects those who are at an advanced stage of the disease for liver transplantation. In this scenario, patients do not necessarily have access to outpatient services and begin to attend them regularly when MELD identifies the advanced stage of the disease, opening a gap between prevention, treatment, and rehabilitation.
- Püschel VAA, Rodrigues AS, Moraes MW. The role of nurses in obtaining organs for transplantation in São Paulo: a legal and bioethical approach. The World of Health Magazine. 2002;26(1).
- Brasil. Law No. 9434 of February 4, 1997. Provides for the removal of organs, tissues, and parts of the human body for transplantation and treatment purposes and contains other provisions. Official Gazette of the Federative Republic of Brazil. Brasília, February 5, 1997; Section 1:2191.
- Andraus W, Haddad L, Rocha-Santos V, D'Albuquerque LAC. Analysis of organ allocation systems for digestive system transplants in Brazil. Medicine (Ribeirão Preto). 2013;46(3):237-42. Available from: https://doi.org/10.11606/issn.2176-7262.v46i3p237-242
- Brazil. Ordinance GM No. 2115 of November 20, 2001. Creates, within the scope of the Secretariat of Health Assistance/National Transplant System, a Working Group with the purpose of studying and suggesting to the Ministry of Health the formulation, review, updating, and improvement of the standards related to the criteria for inclusion of patients who are candidates for liver transplantation in the Single Lists of the states, as well as inclusion criteria for the distribution/allocation of livers collected for transplantation purposes. Official Gazette of the Federative Republic of Brazil, Brasília, 2001. Available from: https://bvsms.saude.gov.br/bvs/saudelegis/gm/2001/prt2115_20_11_2001.html
- Brasil. Ordinance GM No. 541 of March 14, 2002. Approves the criteria for Registration of Liver Recipients – Cadaver Donors, in the Technical Registry of Liver Recipients – “single list” – of the Organ Notification, Procurement and Distribution Centers – CNCDO. Official Gazette of the Federative Republic of Brazil, Brasília. 2005. Available from: https://bvsms.saude.gov.br/bvs/saudelegis/gm/2002/prt0541_14_03_2002.html
- Machado AGS. Impact of implementing the MELD score on liver allocation and liver transplant results: the experience of a Brazilian center. [Dissertation]. [Porto Alegre]: Federal University of Health Sciences of Porto Alegre. 2011;83.
- Brasil. GM Ordinance No. 1160 of 2006. Modifies the criteria for distribution of livers from deceased donors for transplantation, implementing the criterion of severity of the patient's clinical condition. Official Gazette of the Federative Republic of Brazil, Brasília, 2006. Available from: https://bvsms.saude.gov.br/bvs/saudelegis/gm/2006/prt1160_29_05_2006_comp.html
- Moraes ACO, Oliveira PC, Fonseca-Neto OCL. Impact of the MELD score on liver allocation and liver transplant outcomes: an integrated review. ABCD Brazilian Archive of Digestive Surgery. 2017;30(1):65-68. Available from: https://doi.org/10.1590/0102-6720201700010018
- Kamath PS, Wiesner RH, Malinchoc M, Kremers W, Therneau TM, Kosberg CL, et al. Predict survival in patients with end-stage liver disease. Hepatology. 2001;33(2). Available from: https://doi.org/10.1053/jhep.2001.22172
- Wiesner R, Edwards E, Freeman R, Harper A, Kim R, Kamath P, et al. Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology. 2003;124(1):91-96. Available from: https://doi.org/10.1053/gast.2003.50016
- Lombardi AC, Mente ED, Sankarankutty AK, Souza FF, Teixeira AC, Cagnolati D, et al. Analysis of 83 consecutive liver transplants performed at a tertiary care reference hospital in the interior of the state of São Paulo. Acta Cirúrgica Brasileira. 2011;26(6). Available from: https://doi.org/10.1590/s0102-86502011000600020
- Malinis MF, Chen S, Allore HG, Quagliarello VJ. Outcomes among older adult liver transplantation recipients in the Model of End Stage Liver Disease (MELD) Era. Ann Transplant. 2014;19:478-487. Available from: https://doi.org/10.12659/aot.890934
- Mattos AZ, Mattos AA, Sacco FKF, Hoppe L, Oliveira DMS. Analysis of the survival of cirrhotic patients enlisted for liver transplantation in the pre- and post-MELD era in Southern Brazil. Arq Gastroenterol. 2014;51(1). Available from: https://doi.org/10.1590/s0004-28032014000100010
- Sharpton SR, Feng S, Hameed B, Yao F, Lai JC. Combined effects of recipient age and Model for End-Stage Liver Disease score on liver transplantation outcomes. Transplantation. 2014;98(5):557-562. Available from: https://doi.org/10.1097/tp.0000000000000090
- Freitas AC, Shiguihara RS, Monteiro RT, Pazeto TL, Coelho JCU. Comparative study on liver transplantation with and without hepatocellular carcinoma with cirrhosis: Analysis of MELD, waiting time and survival. ABCD Arq Bras Cir Dig. 2016;29(1):21-25. Available from: https://doi.org/10.1590/0102-6720201600010006
- Bajaj JS, Reddy KR, Tandon P, Wong F, Kamath PS, Garcia-Tsao G, et al. The three-month readmission rate remains unacceptably high in a large North American cohort of cirrhotic patients. Hepatology. 2016 Jul;64(1):200-208. Available from: https://doi.org/10.1002/hep.28414
- Billings J, Blunt I, Steventon A, Georghiou T, Lewis G, Bardsley M. Development of a predictive model to identify inpatients at risk of re-admission within 30 days of discharge (PARR-30). BMJ Open. 2012;2(4):1-9. Available from: https://doi.org/10.1136/bmjopen-2012-001667
- Volk ML, Tocco RS, Bazick J, Rakoski MO, Lok AS. Hospital re-admissions among patients with decompensated cirrhosis. Am J Gastroenterol. 2012;107(2):247-252. Available from: https://doi.org/10.1038/ajg.2011.314
- Rosenstengle C, Kripalani S, Rahimi RS. Hepatic encephalopathy and strategies to prevent readmission from inadequate transitions of care. J Hosp Med. 2022;17:S17-S23. Available from: https://doi.org/10.1002/jhm.12896
- Abou-Alfa GK, Jarnagin W, Lowery M, D'Angelica M, Brown K, Ludwig E, et al. Liver and bile duct cancer. In: Neiderhuber JE, Armitage JO, Doroshow JH, Kastan MB, Tepper JE, editors. Abeloff’s Clinical Oncology. 5th ed. Philadelphia, PA: Elsevier; 2014:1373-1395. Available from: https://synapse.mskcc.org/synapse/works/114787
- Patel T, Borad MJ. Carcinoma of the biliary tree. In: DeVita VT, Lawrence TS, Rosenberg SA, eds. DeVita, Hellman, and Rosenberg’s Cancer: Principles and Practice of Oncology. 10th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2015:715-735. Available from: https://mayoclinic.elsevierpure.com/en/publications/cancer-of-the-biliary-tree
- National Comprehensive Cancer Network. Clinical Practice Guidelines in Oncology (NCCN Guidelines®), Biliary Tract Cancers, Version 2.2024. Accessed on 16 August, 2024. Available from: https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1514
- Silva MJ, Rosa MV, Nogueira PJ, Calina F. Ten years of hospital admissions for liver cirrhosis in Portugal. Eur J Gastroenterol Hepatol. 2015;27(11):1320-1326. Available from: https://doi.org/10.1097/meg.0000000000000449
- Armstrong PR, Ring E, MacNicholas R. A decade of rising alcoholic liver disease hospital admissions and deaths in Irish hospitals, 2007-2016: a retrospective cross-sectional analysis. Eur J Gastroenterol Hepatol. 2022;34(6):671-677. Available from: https://doi.org/10.1097/meg.0000000000002339
- Simmons OL, Feng Y, Parikh ND, Singal AG. Primary care provider practice patterns and barriers to hepatocellular carcinoma surveillance. Clin Gastroenterol Hepatol. 2019;17(4):766-773. Available from: https://doi.org/10.1016/j.cgh.2018.07.029
- Moya LC. Spectrum of alcoholic liver disease: a review of pathophysiology and clinical repercussions. Brazilian J Health Rev. 2022;5(4):13904-13927. Available from: https://doi.org/10.34119/bjhrv5n4-159
- Orman ES, Odena G, Bataller RS. Alcoholic liver disease: pathogenesis, management, and novel targets for therapy. J Gastroenterol Hepatol. 2013;1(1):77-84. Available from: https://doi.org/10.1111/jgh.12030
- Sanyal AJ, Bosch J, Blei A, Arroyo V. Portal hypertension and its complications. Gastroenterology. 2008;134(6):1715-1728. Available from: https://doi.org/10.1053/j.gastro.2008.03.007
- Griswold MG, collaborators. Alcohol use and burden for 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease study 2016. Lancet. 2018;392(22):1015-1035. Available from: https://www.thelancet.com/article/S0140-6736(18)31310-2/fulltext
- Billings J, Parikh N, Mijanovich T. Emergency department use in New York City: a substitute for primary care? The Commonwealth Fund. 2000 Nov;(433):1-5. Available from: https://pubmed.ncbi.nlm.nih.gov/11665698/
- Billings J, Parikh N, Mijanovich. Emergency department use: the New York story. The Commonwealth Fund. 2000;(434):1-12. Available from: https://www.commonwealthfund.org/sites/default/files/documents/___media_files_publications_issue_brief_2000_nov_emergency_room_use__the_new_york_story_billings_nystory_pdf.pdf
- Billings J, Parikh N, Mijanovich. Emergency department use in New York City: a survey of Bronx patients. The Commonwealth Fund. 2000;(435):1-5. Available from: https://pubmed.ncbi.nlm.nih.gov/11665700/
- Billings JB, Raven MC. Dispelling an urban legend: frequent emergency department users have substantial burden of disease. Health Aff. 2013;32(12):2099-2108. Available from: https://doi.org/10.1377/hlthaff.2012.1276
- Raven MC, Carrier ER, Lee J, Billings JC, Marr M, Gourevitch MN. Substance use treatment barriers for patients with frequent hospital admissions. J Subst Abuse Treat. 2010;38(1):22-30. Available from: https://doi.org/10.1016/j.jsat.2009.05.009
- An C, Choi YA, Choi D, Paik YH, Ahn AH, Kim M, et al. Growth rate of early-stage hepatocellular carcinoma in patients with chronic liver disease. Clin Mol Hepatol. 2015;21(3):279-286. Available from: https://doi.org/10.3350/cmh.2015.21.3.279
- Debes JD, Chan AJ, Baderramo D, Kikuchi L, Ballerga EG, Prieto JE, et al. Hepatocellular carcinoma in South America: evaluation of risk factors, demographics and therapy. Liver Int. 2008;38(1):136-143. Available from: https://doi.org/10.1111/liv.13502
- Mukthinuthalapati VV, Akinyeye S, Fricker ZP, Syed M, Orman ES, Nephew L, et al. Early predictors of outcomes of hospitalization for cirrhosis and assessment of the impact of race and ethnicity at safety net hospitals. PLoS One. 2019;14(3):e211811. Available from: https://doi.org/10.1371/journal.pone.0211811
- Mendes BC, Oderich GS, Macedo TA, Moreira RK. Ischemic liver lesions mimicking neoplasm in a patient with severe chronic mesenteric ischemia. J Vasc Surg Cases. 2015;1(2):144-147. Available from: https://doi.org/10.1016/j.jvsc.2015.03.020
- Munter BT, Boyd AR, Tchani R, Gray JN, Ramsey PS. Hepatic infarction in pregnancy: a systematic review. Am J Obstet Gynecol MFM. 2024;6(6):1-9. Available from: https://doi.org/10.1016/j.ajogmf.2024.101377