More Information
Submitted: November 19, 2024 | Approved: February 04, 2025 | Published: February 05, 2025
How to cite this article: Nzayikorera J. Fostering Pathways and Creativity Responsible for Advancing Health Research Skills and Knowledge for Healthcare Professionals to Heighten Evidence-Based Healthcare Practices in Resource-Constrained Healthcare Settings. J Community Med Health Solut. 2025; 6(1): 005-019. Available from:
https://dx.doi.org/10.29328/journal.jcmhs.1001052.
DOI: 10.29328/journal.jcmhs.1001052
Copyright license: © 2025 Nzayikorera J. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Evidence-based healthcare; Health research skills and knowledge; Resource-constrained healthcare settings; Healthcare professionals; Creativity and innovation; Developing nations; Africa; Rwanda
Fostering Pathways and Creativity Responsible for Advancing Health Research Skills and Knowledge for Healthcare Professionals to Heighten Evidence-Based Healthcare Practices in Resource-Constrained Healthcare Settings
Janvier Nzayikorera*
Bushenge Hospital, Rwanda
*Address for Correspondence: Janvier Nzayikorera, Bushenge Hospital, Rwanda, Email: [email protected]
Globally, evidence-based healthcare practices are the most dependable framework for effective healthcare decisions and practices. In all nations, financial resources, people, and time are always insufficient. Healthcare professionals should recommend healthcare interventions that have been proven to be safe, effective, and affordable. All healthcare professionals must be creative to be involved in the creation and compilation of trustworthy evidence to support the decrease in morbidity and mortality of communicable and non-communicable diseases, particularly in developing nations. Regretfully, most developing nations still exhibit weaknesses and barriers to promoting health research and evidence-based healthcare. Evidence indicates that developing countries contribute 1% - 2% of health research activities to address global health problems and challenges. As a result, many individuals in these nations continue to have below-average health conditions. The lack of creativity, innovation, and motivation to gain health research competencies for healthcare professionals causes all these issues. Creativity and innovation are the foundations for the effective implementation of evidence-based healthcare. Surprisingly, no researchers have explored how creativity and innovation heighten evidence-based healthcare practices. The primary objective of this project will be to foster pathways and explore the creativity that advances health research abilities among healthcare professionals to improve evidence-based healthcare practices in resource-limited healthcare settings.
Achieving the United Nations Sustainable Development Goals, which include “goal 3: ensure healthy lives and promote wellbeing for all at all ages,” will require greater work and dedication than ever before [1]. One of the best strategies to guarantee everyone’s health and well-being, regardless of country, is to advance science and technology. At the 2020 United Nations High-level political forum session, ministers committed to “strengthening the science-policy interface through evidence-based policymaking, support for research and development, harnessing science, technology, and innovation, and leveraging technologies to promote an inclusive digital economy and resilience across sectors” [2]. However, it is unethical that numerous countries do not sufficiently support the advancement of scientific activities. For instance, “African heads of state and government have committed to raising their national gross expenditure on research and development to at least one percent of their gross domestic product to drive innovation, productivity, and economic growth” [3,4]. However, in Africa, no single country has allocated 1% of its gross domestic product towards scientific research and development. Thus, in Africa, research and development, including health research, are still lagging. Accordingly, all nations should be producers of research as well as consumers. However, evidence indicates that developing countries contribute only 1% - 2% of research activities to help the world solve global health problems and challenges [5]. These are painful facts, given that the majority of developing countries have established health research agendas, as do their academic institutions and health-related associations. Some countries have had those agendas for decades.
Despite notorious long-lasting ineffective health research systems, there have been significant attempts to advance health research in Africa. Institutions like the Global Forum for Health Research have actively supported North-South cooperation, benefiting health research in Africa. The Consortium for Advanced Research Training in Africa (CARTA) aims to build Africa’s local research capacity to understand population health determinants and effectively intervene to improve health outcomes and health systems [6]. It unites a network of nine academic and four research institutions from West, East, Central, and Southern Africa with a few northern universities and training institutes to achieve this ultimate goal. CARTA’s program of operations aims to enhance research infrastructure and capability at African universities and facilitate doctoral training through the establishment of a collaborative program in population and public health. These two goals are interrelated and mutually supportive. Painfully, these programs target seniors working in different academics and health institutions. Most health-related universities of underdeveloped nations teach research methodologies to health-related students. However, the methods used are outdated and incomplete. Upon graduation, the majority of health-related students lack the skills necessary to conduct health research and apply the results of health research. These limitations hinder their ability to fully engage in addressing issues and challenges related to global health. All these factors continue to contribute to the high burden of disease in Africa, both communicable and noncommunicable. In 1990, the Commission on Health Research and Development decreed that strengthening research capacity in low- and middle-income countries is one of the most powerful, cost-effective, and sustainable means of advancing health and development [7–9]. The African Union Development Agency has developed a Health Research and Innovation Strategy for Africa for 2018–2030 [10]. Regretfully, most African nations still exhibit weaknesses, inappropriate strategies, and barriers in terms of advancing evidence-based healthcare practices and ensuring effective health research systems [9]. Likely, as of 2025 Sub-Saharan Africa (SSA), still has worse health indicators than any other region in the world. SSA probably continues to suffer from the 10/90 gap, with developing countries receiving less than 10% of global investments in health research despite accounting for more than 90% of preventable mortality [11,12]. As a result, many individuals in these nations continue to have below-average health conditions. Healthcare professionals in resource-limited healthcare settings lack creativity, innovation, and drive to acquire health research competencies, which causes all these issues. These issues need to be addressed.
A reminder to use evidence-based medicine stems from the 1970s when Dr. Archie Cochrane led a global movement to use substantiated epidemiological information and well-designed research studies, in particular the randomized controlled trial design, to develop effective and efficient diagnostic tools and therapeutic plans [13]. Evidence-based healthcare encompasses every facet of the healthcare industry in every nation. The advent of global ambitions like the Millennium Development Goals, Global Health, and Sustainable Development Goals have accelerated the use of evidence-based healthcare approaches. Universally, such growth has been ongoing and accelerating. From November 17-19, 2008, Bamako/Mali, the global ministerial forum on research for health made a statement that “research and innovation must continue to play a key role in dealing with contemporary health challenges related to the threat of pandemic diseases, increasing importance of chronic diseases, health impacts of climate change, water quality and sanitation, food security, social determinants of health and fragile health systems” [14]. The World Health Organization emphasizes that research evidence and research itself play a crucial role in advancing economic development, health equity, and global health [15]. The strategy for health research was formulated by the sixty-third assembly of the World Health Assembly after a series of assemblies. The approval of this strategy in May 2010 was based on the belief that policies and practices supporting global health should be informed by the best scientific knowledge available. With this strategy, all partners should actively intervene purposefully to harness science, technology, and broader knowledge to create research-based evidence and tools for improving global health. In the forward of Evidence, policy, impact, WHO guide for evidence-informed decision-making, Dr Soumya Swaminathan, a WHO Chief Scientist narrated that “to improve health and well-being and accelerate the achievement of the triple Billion targets, we need better evidence for better decisions” [16]. Health actors have worked hard to actively participate in evidence-based healthcare practices to guarantee effective healthcare strategies. But we need to do much more work to ensure that we effectively and efficiently implement evidence-based healthcare, particularly in developing countries. Probably, Cochrane wanted to help patients in underfunded healthcare settings since he said that money, people, and time would always be insufficient and that healthcare professionals should only recommend healthcare interventions that have been proven to be safe, effective, and affordable. Healthcare stakeholders and players in underdeveloped nations could have improved evidence-based healthcare practices and health research by successfully and efficiently adopting the Cochrane proponent’s ideas. This would have resulted in the preservation of many lives and the implementation of health-maintenance strategies to lower the burden and mortality of various diseases.
Worldwide, approaches to healthcare are always evolving. We need to be creative and come up with new research, medications, and other solutions to keep up with those changes. Creativity is the foundation of innovation. If we do not innovate, the quality of healthcare will not change or advance. Creativity is required to produce knowledge for creating new technologies and advancing research and development. According to Annabel Ten Haven, et al.’s research, creativity is critical for addressing the problems in today’s and tomorrow’s workplaces because it fosters the quest for novel solutions, which are necessary for the quickly evolving healthcare industry [17]. Moreover, according to “Dr Jack Hirsh, Emeritus Professor of hematology and thromboembolism at McMaster University in Hamilton, Ont, and winner of the Canada Gairdner International Award (2000) for excellence in biomedical research, to come up with important questions and find innovative ways of answering them, creativity is a must” [18]. Human beings use a systematizing mechanism (a special circuit in the human brain) to actively seek out various patterns in the world and create something new. With this mechanism, all people have the potential to be creative and innovative. Innovation is one of the strategies to ensure evidence-based healthcare practices. Creativity and innovation can occur at the level of individual healthcare professionals, the healthcare work team, healthcare organizations, or at more than one of these levels combined. In healthcare, there is an increasing need for individuals to generate new ideas and implement them to improve working practices due to the rapid changes taking place [19,20]. Typically, in underfunded healthcare settings, healthcare professionals with diplomas, bachelor’s, and master’s degrees provide healthcare services. However, there have been minimal interventions to ensure these health workers get sufficient knowledge and skills to ensure their effective participation in evidence-based healthcare practices. It is not necessary for those with PhDs; all these healthcare professionals deserve the right to possess maximal competencies to support them in the implementation of evidence-based healthcare. Thus, all initiatives dedicated to enhancing evidence-based healthcare practices should not solely target PhD holders and doctoral training in resource-limited healthcare settings, as has been done over the past years, because these approaches failed to ensure an effective and sustainable health research system. Most PhD holders and those completing doctorate studies in Africa prioritize administrative responsibilities above research; therefore, they don’t often interact with patients. Conversely, healthcare workers who hold diplomas, bachelor’s, and master’s degrees typically interact with patients. Intuitively, all healthcare professionals should have sufficient opportunities to apply creativity and innovation to assist developing countries in optimizing evidence-based healthcare endeavors with the SDGs in effect. Therefore, the methods used to advance health research in Africa need to undergo a drastic and necessary change. To reduce morbidity and mortality from both infectious and noncommunicable diseases, we must consistently urge all healthcare professionals to be creative and innovative in their involvement in the discovery and compilation of reliable evidence. Creativity and innovation are the foundations for the effective implementation of evidence-based healthcare. Surprisingly, no researchers have explored how to use creativity and innovation to heighten evidence-based healthcare practices. The literature gaps indicate that healthcare professionals in resource-limited settings need more studies to foster pathways and explore creativity and innovations that enhance their health research competencies. These studies will help improve evidence-based healthcare practices. This project will address these limitations. This project’s primary objective is to foster pathways and explore the creativity that advances health research abilities among healthcare professionals to improve evidence-based healthcare practices in resource-limited healthcare settings.
Research objectives, questions, methods and research design
We lay out three research objectives (RO1-3), representing independent yet complimentary activities that will contribute to a larger conceptual and empirical framework and an effective health research system in resource-constrained healthcare settings.RO1
To improve the evidence-based healthcare practices for healthcare professionals working in resource-constrained contexts by creating routes and investigating the creativity and innovations that advance quality health research-related educational systems.
Questions
1. How should healthcare practitioners who operate in situations with limited resources rank the strength and longevity of the health research education system they attended?
2. What are the barriers and challenges they faced in terms of obtaining sufficient competencies for pursuing health studies and using health research findings, and do they hope that creativity and innovation will help eradicate those barriers?
3. Does providing those healthcare professionals with the ability to do health research enhance their evidence-based healthcare practices?
Methods
Healthcare professionals working in resource-constrained healthcare settings with diplomas, bachelor’s degrees, and master’s degrees will participate in the study. The research team will conduct a multi-dimensional assessment to measure the quality, sustainability, and barriers of the health research education system they attended. We shall also determine the participants’ pertinent constructs linked to encouraging creativity and innovation to guarantee that healthcare professionals in resource-constrained healthcare settings receive high-quality, long-lasting health research education. Principal component analysis will be used to extract uncorrelated constructs related to barriers and challenges they faced in terms of obtaining sufficient competencies for pursuing health studies and using health research findings and medical professional’s ability to do health research to enhance evidence-based health care practices from an initial set of data on different variables. After determining the underlying constructs, we will reduce the number of variables using exploratory factor analysis. The similar inventiveness and creative constructs that healthcare professionals assert are the routes to removing educational barriers and challenges in acquiring the skills required for pursuing health studies and implementing the findings of health research in resource-constrained healthcare settings will be grouped using cluster analysis techniques. We will use the findings of these analyses in the remaining stages of the project. Next, after completing this survey, the participants will be trained in advanced research methods that could improve evidence-based healthcare practices and health research. Innovatively and creatively, trainers will accomplish health research training using passive, active, constructive, and interactive learning approaches. Passive health research learning will involve watching videos about health research and research techniques. Active health research learning will include learning how to creatively manipulate structural materials to invent knowledge and equipment essential to improving health. Constructive health research teaching will involve encouraging the participants to integrate newly acquired knowledge with what they already know. In interactive health research learning, participants will engage in small group discussions and explore materials, equipment, or devices used in health research like learning how to use statistical software to analyze and present research data. After completing the training, we will conduct another multidimensional survey assessment. We will use paired t-tests to compare the results of this assessment with the previous assessment. Furthermore, we will use conjoint analysis to uncover the most significant attributes and desirable features that define high-quality and sustainable health research-related educational systems for healthcare professionals working in resource-limited healthcare settings.
RO2
Fostering pathways and exploring the creativity and innovations that advance the quality and durable performance of health research activities by healthcare professionals working in resource-limited healthcare settings to improve their evidence-based healthcare practices.
Questions
In what ways can healthcare professionals operating in resource-constrained environments make use of their creative and innovative competency traits to guarantee the long-term and high-quality performance of health research activities to enhance evidence-based healthcare practices?
Methods
A multi-dimensional survey assessment will be employed to investigate participants’ pertinent constructs linked to using creativity and innovative traits to conceptualize and conduct health research studies. Structural Equation Modeling will be used to test and evaluate multivariate causal relationships and to represent how various creative and innovative traits of healthcare professionals working in resource-constrained healthcare settings causally connect in terms of conceptualizing and performing health research studies. Simultaneously, the project steering committee members, lead investigator, and project participants will develop a list of either local, national, continental, or global health problems and challenges that appear to negatively hinder the attainment of well-being and healthy and prosperous lives for the global population. Next, each project participant will choose a problem to work with from such a list. Within six months, using relevant concepts, creativity, and innovation, each participant will develop a research proposal under the mentorship of the project lead investigator and another mentor, if they wish to. The appropriate strategies to address the chosen health problem and challenge shall be included in such a proposal. Upon proposal completion, all proposals will be submitted to the project scientific steering committee to assess and rate the quality, levels of creativity, and innovation that appear in each proposal. The high-quality proposals will be sent to external scientific reviewers to assess and score each proposal on a five-level maturity scale ranging from “weak” to “excellent.” These maturity scales will be characterized as follows: (I) 0-20: Weak; the proposal will require considerable improvement; (II) 21-40: Below average; the proposal will have significant gaps and will require improvement; (III) 41–60: Average; the proposal will be generally accepted at a satisfactory level. (IV) 61–80: Very good; the proposal will be performing at a high level overall, and (V) 81–100: Excellent; the proposal will be performing at the highest level with the capacity to be regarded at global levels. All participants with a proposal score above 41 will be encouraged and supported to pursue research studies on them under the mentorship of the lead investigator. Those with a proposal score below 41 will collaborate with another participant whose proposal has passed.
RO3
Will seek to uncover all techniques to ensure quality and durable utilization of health research findings to improve evidence-based healthcare practices in healthcare settings with limited resources.
QuestionAmong healthcare professionals working in resource-constrained healthcare settings, to what extent are they able to use their creative and innovative competencies to ensure quality and robust utilization of health research findings to improve evidence-based healthcare practices in resource-limited healthcare settings?
Methods
The important constructs of participants’ creativity and innovation traits in terms of using all strategies for the efficient use of literature for evidence-based healthcare will be investigated through the use of a modular and multidimensional survey evaluation. Principal component analysis will be used to extract uncorrelated factors from an initial set of variables. We shall use confirmatory factor analysis techniques to confirm participants’ creativity and innovative traits responsible for advancing health and their research skills and knowledge to heighten evidence-based healthcare practices. After doing such an evaluation, we will create thorough policies, clinical recommendations, and manuals on a few priority diseases in healthcare settings with limited resources by using a structured literature search and the Preferred Reporting Items for Systematic Reviews and Meta-Analysis. We will develop a protocol for inclusion criteria, reporting standards, and data harmonization. To preserve the original context of estimates reported in the literature, the resulting database will include metadata and references to the literature (including specific passages). To create policies, clinical recommendations, and manual documents, we will create data sets, analyze them, and then incorporate the findings into our writings. Those policies, manuals, and clinical recommendation documents shall be submitted to the project’s scientific steering committee to assess and rate the quality, levels of creativity, and innovation that appear in each document. High-quality documents will be sent to outside scientific reviewers, such as international health-related organizations and staff from national ministries of health, to assess and score each document on a five-level maturity scale ranging from “weak” to “excellent.” The following will be used to describe these maturity scales: (I) 0-20: Weak; significant improvement will be needed for the document, (II) 221–40 below average; the documents will have significant gaps and will require improvement; (III) 41–60: Average; a reasonable degree of acceptance will be achieved for the documents; (IV) 61–80: Very good; the document will be performing at a high level overall, and (V) 81–100: Excellent, remarkable documents that will be performing at the highest level and at the pinnacle of their capacity to be acknowledged globally. We shall grant permission to the Ministry of Health or international health-related agencies to adopt any documents that receive a score higher than 61. Moreover, those documents will be submitted to peer-reviewed journals for evaluation and publication.
Study design
We will use three study designs namely: 1) interventional design where participants will receive training, mentorship, and practical sessions; 2) a longitudinal survey (panel and follow-up surveys); and 3) systematic reviews to accomplish research objectives (RO1-3).
Study population, power, and sample size calculation
The project will target healthcare professionals working in Rwanda. Rwanda has about 21,552 registered healthcare professionals. However, all these healthcare professionals will not be used in our study. Estimating the power of a statistical analysis during study planning is a best practice because power analysis helps estimate the minimum required sample size to achieve maximum statistical power for a hypothesized effect size under a specified significance level. Our study will involve Factor Analysis (FA), where sample size is a top priority because FA is essentially based on correlation coefficients. Having adequate statistical power will enable us to observe true relationships in our datasets. Effect size indicates how meaningful the relationship between variables is and indicates the practical significance of research outcomes. The desired power for our study is 0.8. To justify and calculate the required a priori sample size that will produce our desired power, we set the following parameters: 1) Anticipated Effect Size = O.3, 2) Desired Statistical Power Level = 0.8, 3) Number of Latent Variables = 20, 4) Number of Observed Variables = 3 and Probability Levels = 0.5. Using values of these parameters in an a priori sample size calculator for structural equation models, the results are: 1) the Minimum sample size to detect the effect is 227; 2) the Minimum sample size for the model structure is 1,034; and 3) the recommended minimum sample size is 1,034. According to numerous studies, samples above 200 would be enough to detect the effect size and desired power. In this sense, we shall enroll 300 participants.
Sampling techniques
Samples will be drawn from the population using the random sampling technique. Each subject in the population will have an equal and independent chance of being included in the sample. Equal implies that each subject in the population will have the same probability of selection, meaning that other factors like personal preference will not influence a subject inclusion in the sample. Independence means that the choice of one subject will not depend upon the choice of another subject in the sampling; thus, the selection or rejection of one subject will not affect the inclusion or exclusion of another. Random sampling will allow us to obtain a sample that represents the total sampling population. Since our study population is heterogeneous and we need a strong correlation with what we will ascertain, we will use stratified random sampling to obtain the required participants. We will stratify the population based on educational levels to ensure homogeneity within each stratum. Once we have nonoverlapping groups, we will randomly select the required number of participants from each stratum using simple random sampling. Some statistical tests based on the theory of probability will be applied to data collected from random samples. Therefore, the inferences that will be made from such a sample will be generalized to the entire sampling population.
- Age: 18 to 45 years old
- Gender: Male and Female
- Educational level: Diploma, bachelor's degree, and master’s degree
- Nationalities: Any healthcare professionals from any developing nation working in Rwanda shall be eligible.
Exclusion criteria
- Healthcare workers with a PhD degree
- Any healthcare professional who will have enrolled for a PhD degree before the project's initiation.
- Any healthcare professional working in Rwanda who was educated in developed nations.
- Any health worker with non-formal education.
Long-term follow-up and observation sessions: For six years, to track changes among the participants, multiple observations and data collection sessions will be used. Four multidimensional assessments will be used to collect data from participants at different points to observe changes and trends. At the beginning of the study, the first-panel survey will be administered. Other panel and follow-up surveys will be pursued after training, mentorship, and practical sessions about advanced research methods for advancing evidence-based healthcare practices and health research.
Proposed statistical analysis
Sophisticated analysis like Multivariate analysis such as Exploratory Factor Analysis; Confirmatory Factor Analysis Structural Equation Modeling and descriptive statistics such as percentage distribution and shall be used using RStudio, Smart PLS, Jamovi software.
Participants recruitment strategy
To ensure the feasibility of any study, it is crucial to set an effective inclusive participant recruitment strategy. Throughout history and in the present day, various populations have not adequately listened to their needs and demands across all sectors worldwide. Factors such as geographical location have played a role in this lack of attention. Despite saving many lives, healthcare professionals working in rural areas of Africa, often do not receive the necessary support to enhance their health research knowledge and skills. Additionally, women also belong to these underserved groups. To address these issues, participants will be recruited from a wide range of geographical areas, both urban and rural. The first recruitment phase shall include identifying the first 1,000 potential participants. In the second phase, we will randomly sample 300 participants from the pool of 1000 potential participants recruited in the first phase. Some principles that will underpin our participants recruitment shall include:
- Those who meet our study inclusion criteria will be selected without any kind of discrimination.
- Provision of appropriate study information to the participants.
- We shall reasonably approach all participants.
- We shall give compensation to the participants for their participation.
- Participant’s recruitment goals and timeline for recruitment shall be realistic.
- We shall develop an alternative plan for recruitment in case the first plan does not succeed.
- We will use social media, group pages, chat rooms, or discussion boards for digital platforms. Before using this approach, we will ask permission from group or page moderators.
- We will directly recruit potential participants by meeting with them in person and encourage verbally them to join the project.
- Recruitment through community partners and institutions where potential participants are employed will involve sending formal invitations. These invitations will be sent directly to their institutional director or through the Rwanda Ministry of Health or Rwanda Biomedical Center.
Ethical consideration
According to the Helsinki Declaration issued by the World Medical Association in 1964, researchers must ensure and respect the rights, dignity, autonomy, safety, and confidentiality of participants involved in health research [21]. They should design research proposals that uphold the rights and welfare of human participants. Researchers must minimize risks to participants and ensure that the potential benefits of the study outweigh any potential harms. Independent committees like the Institutional Review Board (IRB) or Research Ethics Committee (REC) review research proposals and ensure that research involving human subjects is conducted ethically and complies with legal requirements. IRB may also monitor and review ongoing study activities to ensure that they continue to meet ethical and safety standards. In this study, we opt to respect the dignity, rights, and health of participants 100%. In this sense, we will submit a detailed study protocol and consent form to the Rwanda National Ethics Committee (RNEC) for ethical approval. We will not recruit participants without approval. We will inform the Rwanda Ministry of Health and the Rwanda Biomedical Center in advance about the nature and objectives of our study. Before recruiting participants, we will seek permission from the institutions where those participants work.
Participants and community involvement in the proposal development
- Some will become members of the project advisory board, steering committee, and data management board.
- Some will become members of the research team.
- Some will provide consulting advice to ensure project implementation.
- Some will assist in the recruitment of desired participants.
- Some will remain participants in the project.
- Some will assist in providing training to participants.
- Some will develop cultural sensitivity regarding this project
- They will disseminate project outputs to wider communities using digital platforms
Expected outputs and outcome
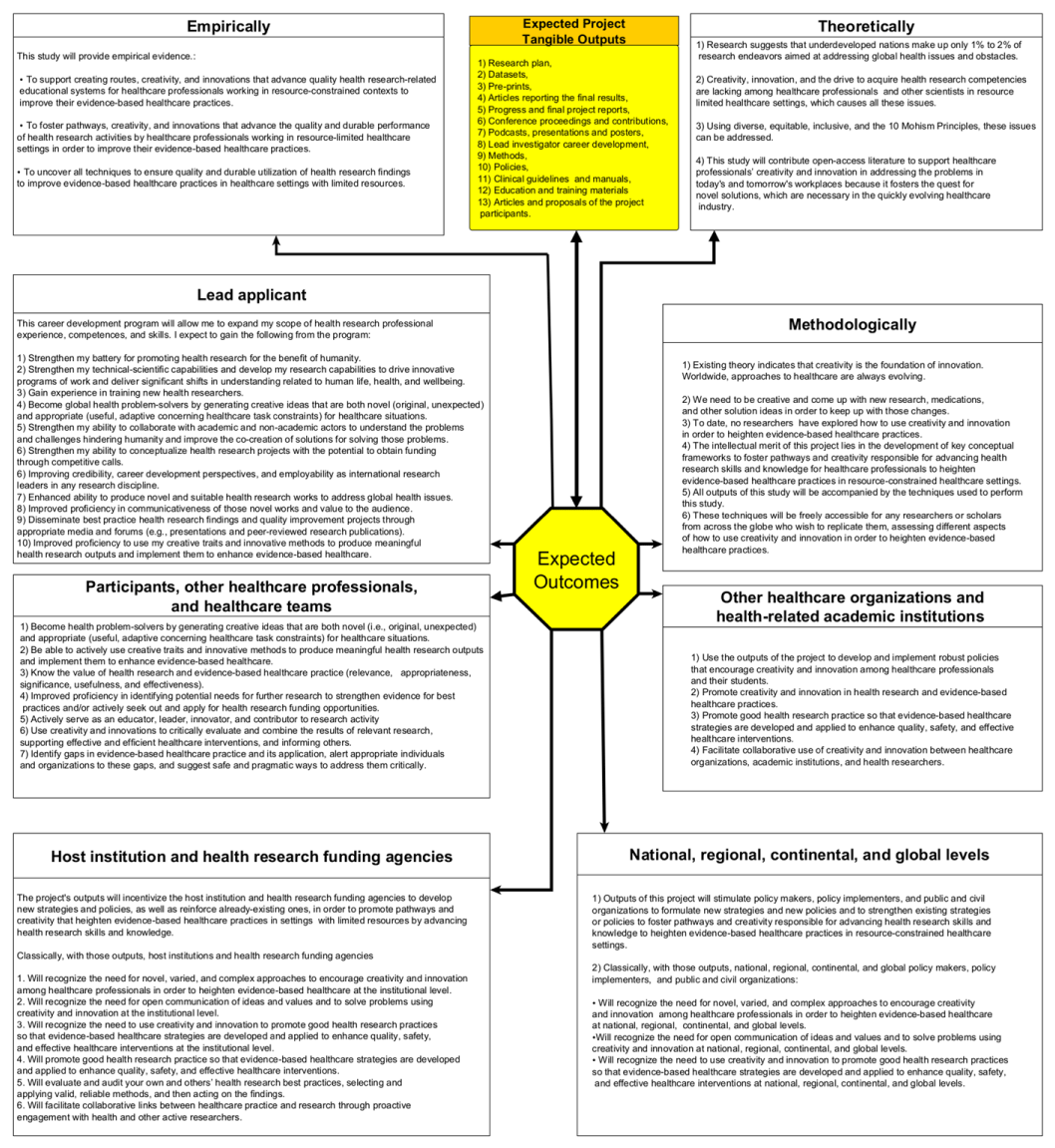
It is anticipated that this research will produce highly original and pertinent outputs and outcomes that will foster pathways and creativity that will advance healthcare professionals’ knowledge and skills in health research, elevating evidence-based healthcare practices in resource-constrained healthcare settings and beyond (Figure 1).
Figure 1: Showing Expected Project Outputs and Outcomes.
Outputs management and sharing
The project outputs will include publications (articles, final project reports, policy reports, clinical guidelines, manuals), datasets, pre-prints, podcasts, webcasts, and conference contributions. Based on the project’s scheduled plan, these outputs will be available at different times. We will use R Markdown or Quarto’s executable notebook formats to compose the project outputs, data, and metadata. We shall adopt open science practices that conform to diversity, equity, inclusion, and the 10 Mohism Principles. There will be no restrictions on sharing data or accessing research output. Mandatorily, progress reports will be available at the end of each year. The progress report will be delivered to funding agencies in plain language, setting out the implications of the results along with a set of observations and suggested policy options. Oral presentations will be scheduled for clarifications and to discuss other relevant project contexts. From the beginning of the project, the project website Oriented to project participants, the academic communities, end users, and other stakeholders will be created. There will be regular updates for the project description, profiles of its participants, and links to all relevant outputs of the project. The findings will be published in pre-print publishing platforms such as SocArxiv, Research Gate, and GitHub repositories with public access. We will publish research outputs in open-access, peer-reviewed journals, whether specialized in health science or multidisciplinary, such as PLOS One and Open Research Europe. 18 research papers, along with final project reports, policy reports, clinical guidelines, and manuals, shall be submitted to open peer-reviewed scientific journals. Among these 18 papers, 6 Research Papers will report the results of objectives (RO1-3). Six papers will report the results, experiences, and milestones gained from the program. Six papers will report relevant concepts and context regarding the broader impacts of career programs. In the end, final reports, policy reports, clinical guidelines, and manuals will be published in research reports, presenting the main research findings in an integrated and synthetic manner, as well as a series of policy options aimed at ensuring stakeholders foster pathways and creativity that advance health research abilities among healthcare professionals to improve evidence-based healthcare practices in resource-limited healthcare settings. Furthermore, as stated in the section is anticipated that 300 papers from projects will be published. For the management of intellectual property, foreseen protection measures, all project outputs will be made available open and freely available under permissive open-source licenses under Creative Commons Attribution 4.0 copyright. For effectively and widely disseminating research outputs, more understandable graphical presentations, podcasts, and helpful maps will be co-designed and presented in workshops and conferences to be attended by health stakeholders and the general public. Oral and written presentations of results shall be addressed to the funding agencies, end users, and policymakers. Yearly, a presentation will be made at the Conference on Public Health in Africa. Presenting the outputs at different seminars, workshops, and conferences will allow the lead investigator to receive criticism and suggestions at an intermediate stage of the project. 84 months will be required to accomplish all these tasks.
Oversight arrangement for the study
The project will establish a scientific steering committee and Data Monitoring Board to safeguard participants’ safety and ensure the appropriateness of project data and outputs. The scientific steering committee shall perform the following tasks, but not be limited to: 1) overall supervising the project; 2) minimizing deviation from the project protocol; and 3) periodically reviewing the progress of the study to assess safety data. 15 members from different countries preferably developing nations shall constitute the project’s scientific steering committee. Members shall not have any financial, scientific, or other competing interests in the project. All potential members will receive an invitation along with the project protocol to comment on before they agree to join the steering committee. Members shall be independent, constructively critical, and supportive of the project objectives and methods. There will be no formal contract between steering committee members and the funding agency. Five members (including the chairman) will constitute a quorum. At some point, the lead applicant and a representative from the funding agency will participate in the committee meetings but will not have voting rights.
The Data Monitoring Board will safeguard the interests of project participants and monitor the data collected from the project, with the authority to modify the data management and monitoring procedures of the protocol. Its role will include but is not limited to: agreeing to and evaluating the data management and project monitoring procedures; assessing recruitment figures and data quality, including completeness; assessing the extent of protocol deviations; informing the steering committee of any major safety concerns; and reviewing the results of the fraud detection procedures. It will consist of five members. Two members will constitute a quorum. Its meetings will take place by teleconference, videoconference, or face-to-face. There will be no formal legal contract between Board members and the funding agency.
The overall structure of the work plan (WP), including deliverables (D) and milestones (M), secondment (S)
WP0: Project Preparation (0 Year)
The objective of WP0 is to ensure efficient project development, transparency, compliance with the norms and standards of scientific practices, and respect for the dignity, rights, and health of human research participants through the following activities: Literature review and completion of project proposal writing (D1). Proposal submission to the funding agencies (M1). Submit proposals to the Institutional Review Board or Research Ethics Committee (M2). Establish the Project Steering Committee (M3). Develop a data management plan (D2). Create the project website (D3). Obtain ethical approval (M4). Planning and recruitment of the participants (M5). Plan and recruit participants (M5). Provide basic information and explain the goals and possible benefits of the projects to participants (M6). Obtaining ethical approval (M4). Providing basic information and explaining to the participants the goals and possible benefits of the projects (M6). Obtaining both verbal and written informed consent from participants (M7).
WP1: Execute activities of Research Objective 1 (RO1) (Year 1, Year 2)
RO1 shall be achieved through the following steps: First Multidimensional Assessment (M8). Survey datasets, data analysis, and manuscript writing (M9). Dissemination of the survey data and manuscript to peer-reviewed journals (D4). Attending the Conference on Public Health in Africa (CPHIA) 2025 and Presenting Survey Results (D5). Providing two years of intensive training for all major advanced research techniques to the participants (M10). Second multidimensional assessment at the end of training (M11). Datasets, data analysis, and manuscript writing for the second survey (M12). Dissemination of the survey data and manuscript submission to the peer-reviewed journal (D6). Attending CPHIA 2026 and presenting the second survey results (D7). Submission of the First (2025) and Second (2026) Progress Reports to funding agencies such as Wellcome Trust (D8). Oral Presentation to the funding agencies for Results Clarifications and Discussion of Other Relevant Project Contexts (D9). Dissemination of the second survey data and manuscripts to peer-reviewed journals (D10). Three months of secondment at Harvard Virtual Training for the lead applicant to obtain a Master of Medical Sciences in Medical Education (S).
WP2: Execute activities of Research Objective 2 (RO2): Year 3, Year 4
RO2 will be achieved through the following steps: Third multi-dimensional survey assessment to investigate participants’ pertinent constructs linked to using creativity and innovative traits to conceptualize and conduct health research studies (M13). Survey datasets, data analysis, and manuscript writing (M14). Dissemination of the third survey data and manuscript to peer-reviewed journals (D11). Attending CPHIA 2027 and Presenting Survey Results (D12). Project steering committee members, the lead investigator, and project participants develop a list of either local, national, continental, or global health problems and challenges (M14). Each participant will choose a problem to work with from such a list (M16). Within six-month periods, the participants will develop a research proposal under the mentorship of the project lead investigator and another mentor, if they wish to (M17). Submission of the proposal to the project scientific steering committee to assess and rate the quality, levels of creativity, and innovation that appear in each proposal (D13). The high-quality proposals will be sent to external scientific reviewers to assess and score each proposal on a five-level maturity scale ranging from “weak” to “excellent (D14). Encouraging and supporting all participants whose proposal score is above 41 to pursue research studies on them (M18). Submission of the third and fourth Progress Reports to the funding agencies (D15). Oral Presentation to the funding agencies for Results Clarifications and Discussion of Other Relevant Project Contexts (D16). Attending CPHIA 2028 and Presenting Survey Results (D17).
WP3: Execute activities of Research Objective 3 (RO3) (Year 5, Year 6)
RO3 will be achieved through the following steps: Fourth multi-dimensional survey assessment to investigate important constructs of participants’ creativity and innovation traits in terms of using all strategies for the efficient use of literature for evidence-based healthcare (M19). Survey datasets, data analysis, and manuscript writing (M20). Dissemination of the third survey data and manuscript to peer-reviewed journals (D18). Attending CPHIA 2029 and Presenting Survey Results (D19). Create thorough policies, clinical recommendations, and manuals on a few priority diseases in healthcare settings with limited resources by using a structured literature search and the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (M21). Submission of those documents to the project’s scientific steering committee to assess and rate the quality, levels of creativity, and innovation that appear in each document (D20). Submission of high-quality documents to outside scientific reviewers to assess and score each document on a five-level maturity scale ranging from “weak” to “excellent.”(D21). Granting permission to the Ministry of Health or an international health-related agency to adopt any documents that receive a score higher than 61 (D22). Submission of those documents to peer-reviewed journals for evaluation and publication (D23). Submission of the fifth and sixth Progress Reports to the funding agencies (D24). Oral Presentation to the funding agencies for Results Clarifications and Discussion of Other Relevant Project Contexts (D25). Attending CPHIA 2030 and Project Results (D26).
WP4: Communication activities and public engagement (Year 1–Year 7)
These will be achieved via the following activities: Yearly delivery of an informative note to the news media about project progress (DE1). Delivery of a quarterly bilingual (Kinyarwanda and English) newsletter and podcast about project progress and creative health research strategies for advancing society (DE2). Regularly update the project website contents. Monthly meetings with the supervisor and mentor to evaluate project progress (DE3).
WP5: Finalizing project activities and disseminating final outputs (Year 7)
These will be achieved via the following activities: Compilation of all project results into a final report (D27). Lead investigator to prepare seven papers (one for each year) to reflect on the experience, milestones, and relevant concepts gained during this career development (D28). Publication of the final report and other project outputs in open-access publishing journals (D29) (Gantt Chart 1) (Tables 1-10).
| Gantt Chart 1: Showing Overall Project Work Plan. | ||||||||
| 0 Year | 1 Year | 2 Year | 3 Year | 4 Year | 5 Year | 6 Year | 7 Year | |
| WPO | D1, D2, D3, M1, M2, M3, M4, M5, M6, M7 | |||||||
| WP1 | M8, M9, M10, D4, D5, D6, D7, D8, S, | M10, M11, M12, D8, D9, D10, | ||||||
| WP2 | M13, M14, M15, M15, MD16, M17, D12, D13, | M18, D14, D15, D16, D17 | ||||||
| WP3 | M19, M20, M21, D18, D19, | M19, M20, M21, D20, D21, D22, D23, D24, D25, D26, | ||||||
| WP4 | DE1, DE2, DE3 | DE1, DE2, DE3 | DE1, DE2, DE3 | DE1, DE2, DE3 | DE1, DE2, DE3 | DE1, DE2, DE3 | ||
| WP5 | D27, D28, D29 | |||||||
| WP: Work Plan. D: Deliverables; M: Milestone; S: Secondment; DE: Deliverable Essential. | ||||||||
| Table 1: Estimated Budget for 7 Year. | |||||
| Cost Type | Number of Staff | Role Name | Annual Salary (USD) | Total 7-Year Cost (USD) | Justification |
| Salary | 1 | Principal Investigator (Janvier Nzayikorera) | $30,000 | $210,000 | The principal investigator's leadership and expertise shall be crucial for project success. |
| Salary | 3 | Research Assistants | $12,000 each | $252,000 | Research assistants will provide critical support in data collection, analysis, and report writing. |
| Salary | 2 | Data Managers | $12,000 each | $168,000 | Data managers shall be essential for ensuring effective data management and analysis. |
| Subtotal Personnel Costs | $630,000. | ||||
| Table 2: Training and continuing professional development. | ||||
| Cost Type | Description | Annual Cost (USD) | Total 7-Year Cost (USD) | Justification |
| Training | Lead Applicant (Janvier Nzayikorera) | $640 | $4,480 | Essential to stay updated with the latest research methodologies. |
| Training | Research Assistants (3) | $640 each | $13,440 | Enhances their research skills and capacity. |
| Training | Data Managers (2) | $640 each | $8,960 | Develops their data management and analysis expertise. |
| Subtotal Training Costs | $26,880 | |||
| Table 3: Archiving and printing. | ||||
| Cost Type | Description | Annual Cost (USD) | Total 7-Year Cost (USD) | Justification |
| Archival Photocopying | $5,000 | $35,000 | Ensures proper storage and accessibility of project outputs. | |
| Printing (Fieldwork) | $1,000 | $7,000 | Supports fieldwork activities and dissemination of materials. | |
| Subtotal Archiving & Printing | $42,000 | |||
| Table 4: Equipment required. | ||||
| Equipment Type | Quantity | Cost per Item (USD) | Total Cost (USD) | Justification |
| HP Pro x360 Fortis Laptops | 100 | $1,000 | $100,000 | Essential for project staff and participants without personal computers. |
| 4K Projectors | 10 | 1500 | $15,000 | Necessary for training and presentations. |
| Boxes of Pens (BIC) | 150 | $10 | $1,500 | Supplies for training and fieldwork. |
| Boxes of Notebooks | 150 | $10 | $1,500 | Supplies for training and fieldwork. |
| Subtotal Equipment Costs | $118,000 | |||
| Table 5: Access charges. | |||
| Description | Annual Cost (USD) | Total 7-Year Cost (USD) | Justification |
| Hospital Assembly Rooms/Conference Halls | $15000 | $105,000 | Required for training sessions. |
| Table 6: Travel and subsistence. | |||
| Description | Annual Cost (USD) | Total 7-Year Cost (USD) | Justification |
| Conference Attendance (CPHIA) & Subsistence | $17,000 | $119,000 | Provides opportunities for learning, networking, and dissemination. |
| Table 7: Fieldwork expenses. | |||
| Description | Annual Cost (USD) | Total 7-Year Cost (USD) | Justification |
| Fieldwork in Rural Areas | $30,000 | $210,000 | Ensures inclusion of healthcare professionals from rural areas. |
| Table 8: Public engagement and patient involvement. | |||
| Description | Annual Cost (USD) | Total 7-Year Cost (USD) | Justification |
| Dissemination of Project Outputs | $10,000 | $70,000 | Ensures broad dissemination of research findings. |
| Table 9: Other costs. | |||
| Description | Annual Cost (USD) | Total 7-Year Cost (USD) | Justification |
| Conference/Seminar Hosting | $5,000 | $35,000 | Engages a wider audience and promotes knowledge sharing. |
| Recruitment, Advertising, Interviewee Travel | $5,000 | $35,000 | Supports the recruitment process. |
| Project-Dedicated Vehicles (2 Land Cruiser V8), their fuel and maintenance fee | $60,000 | $420,000 | Ensures reliable transportation for project activities. |
| Consultancy Fees (Steering Committee, Data Management Board, IRB) | $20,000 | $140,000 | Provides expert guidance and oversight. |
| Subject/Volunteer Expenses (Participant Compensation) | $50,000 | $350,000 | Compensates participants for their time and contributions. |
| Microgrant for project participants | 350,000 | 2,450,000 | Microgrants for project participants will be essential to foster practical involvement, creativity, and innovation, ultimately ensuring evidence-based healthcare practices. |
| Subtotal | $3,430,000 | ||
| Table 10: Summary of the cost (USD). | |
| Category | Total 7-Year Cost (USD) |
| Personnel | $630,000 |
| Training | $26,880 |
| Archiving & Printing | $42,000 |
| Equipment | $118,000 |
| Access Charges | $105,000 |
| Travel & Subsistence | $119,000 |
| Fieldwork | $210,000 |
| Public Engagement | $70,000 |
| Other Costs | $3,430,000 |
| Contingency (5%) | $109,725 |
| Total Estimated Project Cost (USD) | $4,860,605 |
Contingency
A contingency fund shall include unforeseen expenses. A common practice is to allocate 5% - 10% of the total budget. In this case, a 5% contingency would be approximately $107,500.
Creativity and innovation are the foundations for the effective implementation of evidence-based healthcare. Surprisingly, no researchers have explored how creativity and innovation heighten evidence-based healthcare practices. The primary objective of this project is to foster pathways and explore the creativity that advances health research abilities among healthcare professionals to improve evidence-based healthcare practices in resource-limited healthcare settings.
Principle investigator research contributions
Contributions to the Knowledge Generation: As a visionary scientist, I have had great enthusiasm for promoting deductive reasoning, applied science, and technology, as well as multi-, inter-, trans-disciplinary, and intersectoral modes of practice to solve many global problems. From a young age, I’ve been fascinated by science, particularly as it relates to human health. I have been passionate about strengthening health systems globally, especially in developing countries. I actively seek opportunities to contribute to this goal. I’ve dedicated significant time to exploring diverse methodologies and strategies for improving the global healthcare framework. I believe that optimizing these approaches will enhance evidence-based practice, improve quality of life, and ultimately create a healthier world. I have been convinced that collaboration and a pattern-recognition approach to global health challenges and solutions are key to elevating health systems worldwide. My thinking is independent, scientific, and technically driven.
Due to the lack of universal bioethical knowledge and principles, poverty, hunger, diseases, fear, and violence continue to be prevalent globally. Lives do not thrive, human habitats are not safe, resilient, and sustainable, universal literacy is lacking, and there is limited access to quality education, healthcare, and social protection. The assurance of physical, mental, and social well-being remains uncertain. To address these issues, I have set ambitious goals to inspire various ethics and bioethics-related stakeholders to establish comprehensive and equitable decentralized bioethics implementation systems for a brighter future. Such systems should target all people, from individuals to communities, and finally reach the global level. Through this system, we will abolish any old and new challenges that hinder the attainment of healthy and prosperous lives. My initiatives aim to help make the world a worthy and peaceful place for everyone to live. I have called on all nations and global systems to adopt the 10 Mohism principles to support the achievement of sustainable development for all. I have innovatively established the World Advanced Multi-Health Research Initiatives to leverage all ambitions and create a perfect environment to support reaching the world we want with better health for all. WAMHRI aims to reform how health research is done globally. My works [22-27] have sparked changes in health science, healthcare practice, bioethics, and education settings by inspiring people from all over the world to take action.
Contribution to the development of others: On June 30, 2024, I supported a group of students from Vassar University (USA) and the University of Global Health Equity (Rwanda), led by Professor Thomas Parker, to accomplish their fieldwork in Karongi District (Rwanda) at the KOPAKAMA Cooperative. In a technical capacity, I have helped many students from many universities finish their dissertations, research proposals, and other assignments that call for technical writing proficiency. Around 1500 scholars and students from all over the world have invited me to join them in pursuing research projects and building partnerships, however, time and resources would not allow me to join them all. The majority of them have asked me to teach them statistical software packages and technical scientific communication techniques through our collaboration. More than 1000 readers of my work and blog have given me feedback. Enthusiastically all of them have developed motives to advance bioethics for the benefit of others. After learning about my published papers, several international scientific conference organizers encouraged me to participate as a delegate.
Contribution to a wider research community: I, as a visionary scientist, have great enthusiasm to ensure inclusive and dynamic growth and development of the research community worldwide. Some of my contributions are as follows: 1) blog Peer Reviewer of National Institute for Health and Care Research (NIHRI), 2) a member of International Network for Government Science Advice (INGSA), 3) a Blog Writer for Global Development Network (GDN), 4) editorial member of Biomedical Research Clinical Advancement, 5) an associate Editor member of Journal of Medical Case Studies (JMCS), 6) an article Peer Reviewer of European Medical Journal (EMJ), 7) an article Peer Reviewer of Archives of Current Research International, 7) a Guest Editor of Cureus, 8) article peer reviewer of Asian Journal of Research in Nephrology, 9) an abstract reviewer for the World Federation for Medical Education (WFME) Conference 2025. 10) Contributor to the WFME’s Declaration on Institution’s Responsibility to Support Medical Students, Physicians in Postgraduate Education, and Physicians in Practice. Numerous esteemed scientific publishing journals have requested that publish my works with them and become an editorial member of their journals; however, time and resources would not allow me to join them all.
I have published in journals that follow the Creative Commons Attribution-Non-Commercial 4.0 License. I have volunteered to provide content to the International Network for Government Science Advice (INGSA). I proposed to the INGSA Africa chapter to organize certain events that empower young scientists to use scientific facts and approaches in line with the 10 Mohism Principles to support achieving sustainable development goals in their nations. I have actively given my criticism about how things should be done by attending numerous conferences. For example, during the Conference of the Parties (COP28), I proposed a need to amend the term “climate change” to “abnormal climate change”. I have participated in various research projects as a data analyst, project designer, and research respondent, for instance, I took part in the survey named “UNESCO’s Global Call for Best Practices in Open Science.” My genuine contributions to enhancing research culture—including research integrity, equity, diversity, and researcher mobility—come from the founding of WAMHRI.
Contribution to a positive and inclusive research culture: This proposal is relevant to all of my previous research activities that have centered on health and bioethics. Bioethics is a realm of wisdom; in fact, it is a bridge to the future because it entails teaching people how to use knowledge for human survival and improvement in the quality of life. As an aspiring revolutionary health researcher seeking a tenure-track position to lead substantial and innovative research programs universally, having bioethics knowledge will support me in building my career goals, expanding my scope of experience, and supporting a positive and inclusive research culture through mentoring, supporting collaboration and interdisciplinarity, leadership and people management, and promoting research integrity. The project will focus on enhancing and exploring the extent of using creativity and innovation to heighten evidence-based healthcare practice in resource-limited healthcare settings as a way of improving human survival and quality of life. To ensure inclusiveness, we will also recruit underserved groups, such as women and healthcare professionals working in rural areas, as participants in the project. We will not allow any kind of discrimination throughout this project. I will enroll at Harvard for the three-month course where I will receive intensive training and work on how to maximize collaboration and interdisciplinarity projects in leadership and people management in health research. I will teach participants how to conceptualize, conduct, and evaluate health research projects using hands-on and theoretical-based approaches. To promote research integrity, we will use ethical theories such as consequentialism, deontology, and virtue ethics, and also bioethical principles, namely justice, nonmaleficence, beneficence, and autonomy, to empower project participants to safeguard and respect their rights, dignity, and health and of other people. Furthermore, we will train participants on how to avoid research misconduct, such as fabricating data, falsifying research materials or altering data, and plagiarizing someone else’s work without giving credit. Participants shall stay away from these unethical practices. To ensure a positive and inclusive research culture, we will empower our project participants to sign and abide by the DORA declaration. This declaration encourages all individuals and organizations interested in developing and promoting best practices in assessing scholarly research to be positive. Essentially this program will turn me into a highly trained health research scientist. Thus, I will continue to provide mentorship and consultation to various scholars who are passionate about advancing the fields of health science, healthcare, and health research. I will also host a workshop, design tutorials, and develop training materials to teach advanced techniques used in health research. Future directions for my research include (I) investigating local and regional impacts of using evidence-based healthcare practices for effective management of non-communicable disease and communicable disease in Africa; (II) using creativity and innovative approaches to forecast dynamic trends in the management of non-communicable and communicable disease; and (III) developing a creativity and innovation framework for strengthening health research in Sub-Saharan Africa. The participants of this project and other health scientists shall be invited to join me in these projects to strengthen my collaborative, knowledge-creation, and interdisciplinarity practical approaches.
Research environment
From applicant to the host: It is genuinely important to enhance health research for the benefit of humanity. The World Advanced Multi-Health Research Initiatives (WMHRI) aim to be a unified, global multidisciplinary, non-government, non-profit health research organization dedicated to promoting and advancing health research for the benefit of humanity. More than ever, our societies need people with critical minds—people who can look at health research, ask their own questions, and find their answers—thereby, in turn, supporting healthcare practical-related decisions and health policy formulation and thus helping to solve global health problems or challenges.” By embracing this claim, healthcare professionals can foster pathways and creativity that advance their skills and knowledge in health research, ultimately enhancing evidence-based healthcare practices in resource-constrained settings. Therefore, I have decided to pursue my research activities with WAMHRI. I believe that my work will provide creative and innovative approaches to WAMHRI to help it achieve some of its mandates.
From host institution to the applicant: Working with WAMHRI will enable me to develop my research identity and explore my research questions more effectively. This is because WAMHRI focuses on teaching advanced techniques for health research, using these techniques for basic and applied research, and promoting the thorough use of research findings in healthcare decision-making and policy formulation. Additionally, working with WAMHRI will help me strengthen my leadership and management skills, as the organization prioritizes principles of good governance such as accountability, leadership, integrity, stewardship, transparency, consensus-building, equity, and inclusion. Therefore, I will actively engage in avoiding any kind of malpractice, including financial malpractice (such as fraud, corruption, bribery, coercion, collusion, money laundering, modern slavery, facilitation of tax evasion, and financing terrorism), and discrimination that hinders the progress of health research and other fields.
Contribution (training and continuing professional development) of the host organization to the staff employed on gran: the World Advanced Multi-Health Research Initiatives will provide staff with a minimum of 10 days per year to work with applicants. We will make use of this time to make sure the project is carried out effectively and efficiently. We will motivate project participants to actively engage in implementing various proclamations and policies that support prosperity, well-being, and a healthy lifestyle. We will foster pathways and creativity to advance health research skills and knowledge for healthcare professionals, leading to heightened evidence-based healthcare practices in resource-constrained healthcare settings. The Health Research and Innovation Strategy for Africa (HRISA) 2018–2030, the Rwanda Health Sector Research Policy, the Africa Health Strategy 2016–2030, and the Bamako call to action on research for health research are a few of these statements and policies. By doing this, a positive research culture will be fostered. We will use this time as part of people management to enable project participants to perform at their best and foster a culture of trust, respect, and collaboration in the healthcare and health research communities. We’ll do this by creating a culture that is upbeat, productive, and disciplined; by developing close bonds with participants; by giving them the tools and resources they require; and by supporting their professional and skill development. We will also take advantage of this time to participate in open science, making sure that we produce transparent and easily readable knowledge via cooperative networks that support inclusion, equity, and diversity in the field of health research. All of these actions will support the building of an effective and larger conceptual and empirical framework and an effective health research system in resource-constrained healthcare settings.
- United Nations. 2030 Agenda for Sustainable Development. Sustainabledevelopment.un.org [Internet]. 2016 [cited 2025 Feb 4]. Available from: https://www.un.org/ohrlls/sites/www.un.org.ohrlls/files/2030_agenda_for_sustainable_development_web.pdf
- UN DESA. CEPA Strategy Guidance Note on the Science-Policy Interface. UN [Internet]. 2021 Mar [cited 2025 Feb 4]. Available from: https://ingsa.org/knowledge-hub/reports/
- Africa UNEC for. NTIS Policy Brief Draft: Realizing the R&D Expenditure Target of "1% of GDP". 2023 [cited 2025 Feb 4]. Available from: https://au.int/sites/default/files/decisions/9526
- Hedt-Gauthier BL, Jeufack HM, Neufeld NH, Alem A, Sauer S, Odhiambo J, et al. Stuck in the middle: A systematic review of authorship in collaborative health research in Africa, 2014–2016. BMJ Glob Health. 2019;4(5):e001853. Available from: https://gh.bmj.com/content/4/5/e001853
- Rahman MM, Ghoshal UC, Ragunath K, Jenkins G, Rahman M, Edwards C, et al. Biomedical research in developing countries: Opportunities, methods, and challenges. Indian J Gastroenterol. 2020 Jun;39(3):292-302. Available from: https://doi.org/10.1007/s12664-020-01056-5
- Ezeh AC, Izugbara CO, Kabiru CW, Kahn K, Manderson L, Undieh AS, et al. Building capacity for public and population health research in Africa: The Consortium for Advanced Research Training in Africa (CARTA) model. Glob Health Action. 2010;3. Available from: https://doi.org/10.3402/gha.v3i0.5693
- Franzen SR, Chandler C, Lang T. Health research capacity development in low and middle-income countries: Reality or rhetoric? A systematic meta-narrative review of the qualitative literature. BMJ Open. 2017 Jan 27;7(1):e012332. Available from: https://doi.org/10.1136/bmjopen-2016-012332
- Evans R J. Health Research Essential Link to Equity in Development. Oxford (New York, Toronto): Oxford University Press; 1990. Available from: https://www.ncbi.nlm.nih.gov/books/NBK209096/
- Jones MC. Strengthening national health research systems in Africa: Lessons and insights from across the continent. London: LSE Health. 2021 [cited 2025 Feb 4].
- African Union Development Agency (AUDA)-NEPAD. Health Research and Innovation Strategy for Africa (HRISA) 2018-2030. African Union Development Agency (AUDA)-NEPAD. 2019 [cited 2025 Feb 4]. Available from: https://www.nepad.org/publication/health-research-and-innovation-strategy-africa-hrisa-2018-2030
- Currat LJ, Francisco A De, Nchinda TC. The 10/90 report on health research. Davey S, editor. Geneva: Global Forum for Health Research; 2000. Available from: https://www.files.ethz.ch/isn/20413/10.90.FULLTEXT.pdf
- Kilama WL. The 10/90 gap in sub-Saharan Africa: Resolving inequities in health research. Acta Trop. 2009;S8-S15. Available from: https://doi.org/10.1016/j.actatropica.2009.08.015
- Sullivan BM. Introduction to evidence-based practice at National University of Health Sciences. Natl Univ Heal Sci [Internet]. 2009 [cited 2025 Feb 4];1–16. Available from: https://www.nuhs.edu/media/25290/tutorial-intro_to_ebp.pdf
- The Lancet. The Bamako call to action: research for health. Lancet. 2008 Nov 29;372(9653):1855. Available from: https://doi.org/10.1016/s0140-6736(08)61789-4
- World Health Organization (WHO). The WHO strategy on research for health. WHO Libr Cat Data. 2012. Available from: https://www.afro.who.int/sites/default/files/2020-11/WHO_Strategy_on_research_for_health.pdf
- World Health Organization (WHO). Evidence, policy, impact. Geneva: World Health Organization; 2021.
- Haven A, Pragt E, Luijk SJ Van, Diana HJM, Mook WNKA Van, Pragt E, et al. Creativity: A viable and valuable competency in medicine? A qualitative exploratory study. Med Teach [Internet]. 2022;44(10):1158–64. Available from: https://doi.org/10.1080/0142159X.2022.2072278
- Fleet R. On creativity and innovation. Can Fam Physician. 2014;60(10):950-951. Available from: https://pubmed.ncbi.nlm.nih.gov/25316752/
- Patterson F, Zibarras LD. Selecting for creativity and innovation potential: Implications for practice in healthcare education. Adv Heal Sci Educ. 2017;22(2):417–28. Available from: https://doi.org/10.1007/s10459-016-9731-4
- Zuber C, Moody L. Creativity and innovation in healthcare: Tapping into organizational enablers through human-centered design. Nurs Adm Q. 2018;42(1):62-75. Available from: https://doi.org/10.1097/naq.0000000000000267
- World Health Organization (WHO). Declaration of Helsinki: World Medical Association Declaration of Helsinki. WHO. 2001;79(June 1964).
- Janvier N. Hazardous effects of malaria for patients residing in low-probability malaria areas: A case report and critiques of the literature for cerebral malaria. J Community Med Heal Solut. 2023;4(2):076-079. Available from: https://www.communitymedjournal.com/apdf/jcmhs-aid1038.pdf
- Janvier N. Healthcare bioethics: A vital branch of bioethics and a new possible pillar for modern healthcare systems strengthening worldwide. J Community Med Heal Solut. 2023;4(2):063-075. Available from: https://www.communitymedjournal.com/apdf/jcmhs-aid1037.pdf
- Nzayikorera J. Existence of unequal treatment in healthcare: An indicator for the violation of healthcare bioethical principles. Glob Bioeth Enq. 2023;11(June 1993):12–27. Available from: https://doi.org/10.38020/GBE.11.1.2023.12-27
- Janvier N. African countries being categorized as developing countries should not be an excuse for having a weak/poor health system. 2022;10(5):2119–24.
- Nzayikorera J. Complications and avoidance of the complications associated with management of abdominal trauma. In: Garbuzenko DV, editor. Abdominal Trauma - New Solutions to Old Problems [Internet]. UK: IntechOpen; 2023. Available from: https://www.intechopen.com/chapters/83215
- Nzayikorera J. The development of bioethics: Historical facets vital in the foundation and development of healthcare bioethics. Glob Bioeth Enq [Internet]. 2023;11:155–71. Available from: https://www.researchgate.net/profile/Janvier-Nzayikorera/publication/380902251_Janvier_The_Development_of/links/6654b2efbc86444c72072cfa/Janvier-The-Development-of.pdf