More Information
Submitted: December 18, 2024 | Approved: January 06, 2025 | Published: January 07, 2025
How to cite this article: Makalo L, Perez OR, Martin B,Jallow CS, Jobarteh ML, Baldeh A, et al. Case Report: Intussusception in an Infant with Respiratory Syncytial Virus (RSV) Infection and Post-Operative Wound Dehiscence. J Community Med Health Solut. 2025; 6(1): 001-004. Available from:
https://dx.doi.org/10.29328/journal.jcmhs.1001051.
DOI: 10.29328/journal.jcmhs.1001051
Copyright license: © 2025 Makalo L, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Intussusception; Respiratory syncytial virus; RSV; Paediatric; Wound dehiscence; Surgical complications; Postoperative care
Case Report: Intussusception in an Infant with Respiratory Syncytial Virus (RSV) Infection and Post-Operative Wound Dehiscence
Lamin Makalo1,2*, Orlianys Ruiz Perez1, Benjamin Martin3, Cherno S Jallow2,3, Momodou Lamin Jobarteh1, Alagie Baldeh3, Abdul Malik Fye3, Fatoumatta Jitteh1 and Isatou Bah1
1Department of Paediatrics, Edward Francis Small Teaching Hospital, Banjul, The Gambia
2School of Medicine and Allied Health Sciences, University of The Gambia, The Gambia
3Department of Surgery, Edward Francis Small Teaching Hospital, Banjul, The Gambia
*Address for Correspondence: Dr. Lamin Makalo, Department of Paediatrics, School of Medicine, University of The Gambia, Banjul, The Gambia, Email: [email protected]
Intussusception is a leading cause of intestinal obstruction in young children, typically presenting with colicky abdominal pain and altered stool characteristics, before progressing to abdominal distension and bilious vomiting. This case report describes an 8-month-old male who presented with gastrointestinal symptoms, respiratory distress, and signs of intestinal obstruction. The patient was diagnosed with intussusception and found to be positive for Respiratory Syncytial Virus (RSV). After an attempted ultrasound-guided hydrostatic fluid enema, he underwent laparotomy to resolve the intussusception but developed post-operative complications, including delayed wound healing and wound dehiscence. The interplay of viral infections like RSV, and treatments such as steroids in pediatric surgical cases warrants further attention, especially concerning postoperative outcomes.
Intussusception is a common pediatric emergency, particularly in infants and children under two years of age, and is characterized by the telescoping of one segment of the bowel into another [1]. Respiratory Syncytial Virus (RSV) infection is typically associated with respiratory symptoms but can also present with gastrointestinal disturbances [2,3]. In this case, an 8-month boy who presented with both gastrointestinal and respiratory symptoms, was diagnosed with intussusception and subsequently developed post-operative wound dehiscence after laparotomy. This report highlights the importance of recognizing the factors that could contribute to such complications in the management of pediatric surgical cases complicated by viral infections.
An 8-month-old male infant was admitted to the Emergency Pediatric Unit with a 3-day history of rhinorrhea, loose watery stools that became bloody on the second day, vomiting, cough, and abdominal distention. He was a full-term baby, delivered via spontaneous vaginal delivery at 38 weeks of gestation, with a birth weight of 3.4 kg. He had been progressing normally with exclusive breastfeeding until 6 months of age when supplementary feeding with Lactogen® was introduced.
On examination, the infant was found to be pale, moderately dehydrated, and afebrile (36.7 °C). The patient exhibited subcostal and intercostal retractions, along with rhonchi on auscultation, indicative of respiratory distress. On abdominal examination, abdominal distention and tenderness were present, and a palpable mass in the right upper quadrant suggested a possible obstructive etiology.
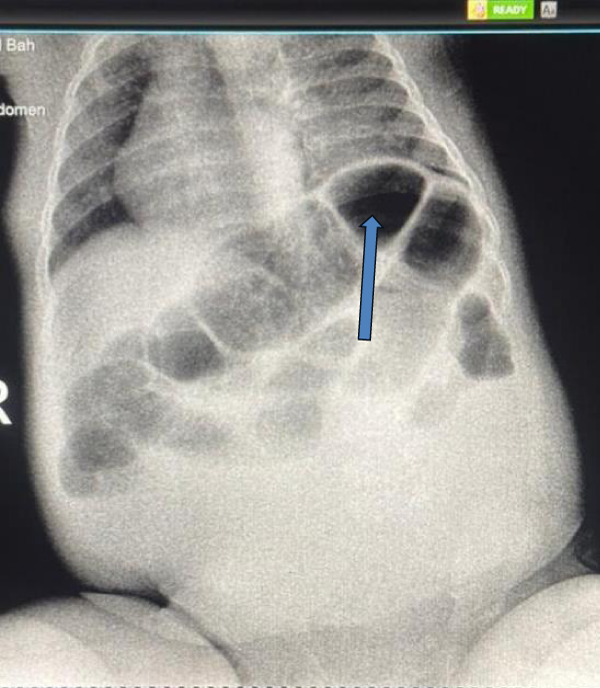
A stool examination revealed bloody stools by the third day of symptom onset. Laboratory results showed a leukocyte count of 6.8 × 109/L and hemoglobin of 7.8 g/dL (indicating moderate anemia). Mild hypokalemia of 3.06 mmol/L was noted, likely due to vomiting. A rapid point-of-care diagnostic test for Respiratory Syncytial Virus (RSV) was positive, confirming the viral etiology for the respiratory symptoms. Erect abdominal X-ray showed signs of intestinal obstruction, including dilated bowel loops and air-fluid levels, raising suspicion for intussusception (Figure 1). A diagnostic ultrasound confirmed the diagnosis.
Figure 1: Abdominal X-ray showing signs of intestinal obstruction (dilated bowel loops, air-fluid levels-arrow).
The patient was taken to radiology to attempt an ultrasound-guided hydrostatic enema, but no process was made and the tip of the intussusceptum was seen to be in the descending colon in the left iliac fossa. The patient underwent further resuscitation with intravenous fluids and provided gastric decompression via a nasogastric tube while the patient was prepared for surgery. The anesthetic review noted the concurrent lower respiratory tract infection, and the potential challenge for extubation, but due to the emergent nature of this condition and the potential for bowel ischaemic, surgical management was the only management option for the patient. The surgical procedure involved general anesthesia and endotracheal intubation. A transverse upper abdominal incision was used, revealing a segment of the ileum telescoping into the cecum and ascending colon, with gangrenous ileum and coincidental malrotation. The intussuception could not be reduced manually, and so a limited right hemicolectomy was performed meaning the operation was classed as clean-contaminated [4]. The abdomen was closed in three layers by a consultant pediatric surgeon, and the patient was closely monitored in the postoperative period.
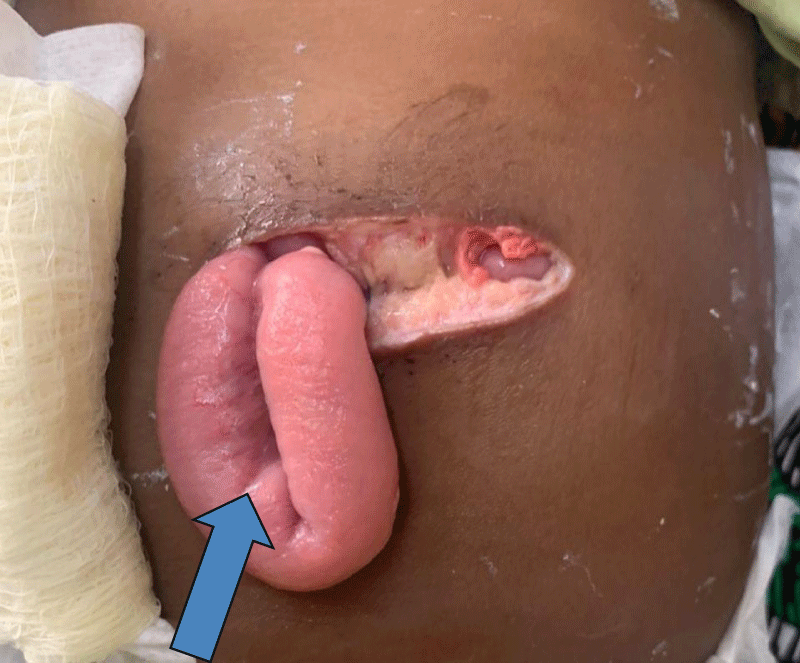
Postoperatively, the child’s recovery was complicated by delayed wound healing and subsequent wound dehiscence (Figure 2). On the ninth day after surgery, the surgical wound showed signs of poor healing, and a small portion of the incision broke down completely leading to a small bowel protruding from the surgical site. Although infection was considered, no overt signs of purulent drainage or systemic infection were noted. The dehiscent wound was closed in layers, with non-absorbable skin sutures, by a surgical resident, and daily dressing changes, along with close monitoring for infection were initiated. The patient was continued on intravenous antibiotics as a precaution and nutritional support was adjusted with enteral feeds as tolerated. Despite the resolution of respiratory symptoms, the child’s bowel was again noted to be protruding from the surgical wound by the fifteenth day, and the dehiscent wound was closed again. This time absorbable sutures were used for the thin and retracted muscle layer, and non-absorbable mass closure sutures were used for the muscle/fat/skin.
Figure 2: Protruding small bowel from the surgical wound due to full-thickness wound dehiscence (arrow).
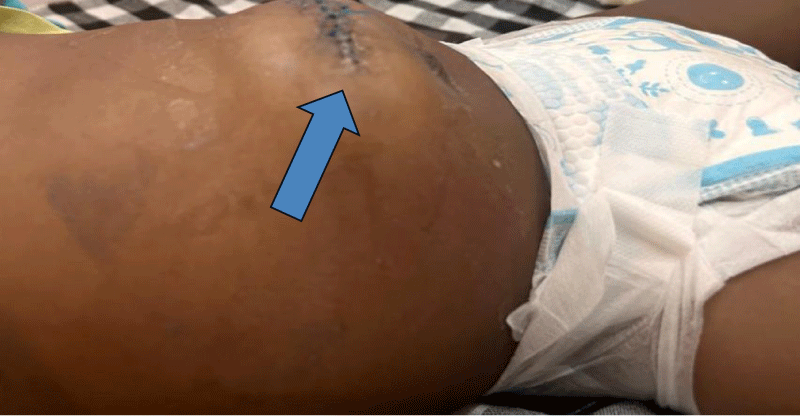
Despite these complications, the patient showed gradual improvement over the following week. The wound edges were approximated, but an incisional hernia was evidence, which would require further surgical intervention. The patient was discharged on the 22nd postoperative day for both pediatric and pediatric surgical follow-up (Figure 3).
Figure 3: Postoperative healing with incisional hernia (arrow).
At discharge, the infant was feeding well, with no further signs of gastrointestinal or respiratory distress. Follow-up visits were planned for two weeks and one month postoperatively, and no further complications related to the RSV infection were noted.
This presentation emphasizes the complexity of the case, involving both respiratory and gastrointestinal symptoms that required surgical intervention, as well as postoperative complications linked to the patient’s viral infection. The detailed timeline of care, including diagnostic steps, surgical management, and recovery process, provides a comprehensive overview of the patient’s hospital course.
Intussusception in infants typically presents with the classic triad of abdominal pain, vomiting, and bloody stools [4-6]. This case highlights an unusual but important aspect of intussusception: the potential for concurrent or even causative viral infections, such as RSV, to complicate the clinical picture. While RSV is primarily associated with respiratory distress, this case illustrates its association with gastrointestinal symptoms, such as vomiting and diarrhea, which may delay the diagnosis of intussusception [2]. A similar case was reported in America by Moore and Berne, et al.
in 2006, which also noted the association between RSV and gastrointestinal disturbances [7]. Additionally, other studies have documented the presence of RSV in the gut and its link to various gastrointestinal pathologies, suggesting that RSV infection may play a role in disrupting the normal function of the gut, potentially contributing to the development of conditions like intussusception [8,9].
Intussusception itself can occur due to several lead points including enlarged lymphatic tissue due to viral infections as well as separate pathologies like polyps and Meckel’s diverticulum [10]. The mechanism behind this may involve viral infections like RSV altering the immune response in the gastrointestinal tract, leading to hyperperistalsis, which can facilitate the telescoping of one bowel segment into another [11,12]. One study speculated that RSV infection disrupts the steady state of intestinal bacteria, which results in an imbalance between Th1/Th2 and Treg/Th17 immune cells. This imbalance can contribute to an abnormal immune response in the gut, which may increase the likelihood of intussusception and other gastrointestinal complications. This mechanism could be particularly relevant in the context of viral infections, which can induce systemic inflammatory responses that affect both the respiratory and gastrointestinal systems [13].
Furthermore, research in animal models has shown that RSV can disrupt lung immunity and alter gut microbiota composition. A study involving suckling mice revealed that IL-22 might be the link between lung inflammation and gut dysfunction. The study found that RSV-induced inflammation in the lungs disrupts the development of Th17/Treg cells, leading to altered gut microbiota composition through IL-22-induced overexpression of RegIIIγ [13]. This cascade of immune reactions leads to intestinal immune injury and disruption of normal gut functions, which could predispose to conditions like intussusception.
The successful reduction of intussusception via laparotomy remains the standard treatment when non-surgical methods, such as air/fluid enema reduction, fail. However, postoperative complications, such as wound dehiscence, should be considered, particularly in patients with underlying viral infections like RSV. These infections can alter immune responses, potentially affecting the healing process and leading to complications such as delayed wound healing and wound dehiscence [14]. The delayed wound healing observed in this patient may have been influenced by the systemic effects of RSV. One study found that RSV infection can delay reepithelialisation by attenuating epithelial cell migration, a critical step in wound repair. It also promotes stress fiber formation and mediates the assembly of large focal adhesions [15,16]. This highlights the importance of vigilant postoperative care in these cases, including close monitoring for wound complications and ensuring regular follow-up to ensure full recovery.
This case highlights the importance of considering both gastrointestinal and respiratory etiologies when evaluating pediatric patients with gastrointestinal distress. Intussusception should remain a high differential in infants with abdominal pain, vomiting, and altered stool patterns, even when viral respiratory symptoms are present. Additionally, viral infections like RSV may complicate postoperative recovery, as seen in the delayed wound healing and wound dehiscence observed in this patient. Early identification and management of such complications are crucial for optimal patient outcomes.
Ethical declaration
Ethical approval for this study was obtained from the Research Ethics Committee of the Edward Francis Small Teaching Hospital (EFSTH) in Banjul, The Gambia, IRB No. EFSTH-REC-2024-147. The investigator explained the purpose and objectives of the study to the parents in a language they understood. Written informed consent was obtained from the participants, with the study’s scope, purpose, and benefits clearly explained to the parents. The identities of all participants were kept confidential.
We would like to thank the medical and nursing staff for their assistance in the care of the patient and the surgical team for their expertise in managing this case.
Source of funding: Self-funded.
- Alnamshan M, Almatroudi D, ALmutairi D, Almagushi NA, Almadhi L, Alenazi AM. Idiopathic intussusception in infants and children: Different outcomes in relation to interventions. Cureus. 2023;15(10):e48026. Available from: https://doi.org/10.7759/cureus.48026
- Jiang MY, Duan YP, Tong XL, Huang QR, Jia MM, Yang WZ, et al. Clinical manifestations of respiratory syncytial virus infection and the risk of wheezing and recurrent wheezing illness: A systematic review and meta-analysis. World J Pediatr. 2023;19(11):1030-1040. Available from: https://doi.org/10.1007/s12519-023-00743-5
- Murdoch Childrens Research Institute. Common viruses trigger most cases of intussusception in children. ScienceDaily. 2024. Available from: www.sciencedaily.com/releases/2024/03/240314122131.htm
- Tesfaye DD, Adem BM, Ketema I, Mehadi A, Eshetu B, Teshager T, et al. Clinical profile and treatment outcome of acute intussusception among children in eastern Ethiopia: A seven-year retrospective study. Front Pediatr. 2022 Nov 28;10:968072. Available from: https://doi.org/10.3389/fped.2022.968072
- Madan AJ, Haider F, Alhindi S. Profile and outcome of pediatric intussusception: A 5-year experience in a tertiary care center. Ann Pediatr Surg. 2021;17:31. Available from: https://doi.org/10.1186/s43159-021-00097-5
- Wu TH, Huang GS, Wu CT, Lai JY, Chen CC, Hu MH. Clinical characteristics of pediatric intussusception and predictors of bowel resection in affected patients. Front Surg. 2022;9:926089. Available from: https://doi.org/10.3389/fsurg.2022.926089
- Moore FO, Berne JD, Slamon NB, Penfil SH, Dunn SP. Intussusception in a child with respiratory syncytial virus: A new association. Del Med J. 2006;78(5):185-7. Available from: https://pubmed.ncbi.nlm.nih.gov/16739938/
- Okada T, Matsubara K, Matsushima T, Komiyama O, Chiba N, Hamano K, et al. Analysis of clinical features of community-acquired pneumonia caused by pediatric respiratory syncytial virus and human metapneumovirus. Kansenshogaku Zasshi. 2010;84(1):42-7. Available from: https://doi.org/10.11150/kansenshogakuzasshi.84.42
- Sallam M, Breuer R, Wrotniak B, Alibrahim O. Necrotizing enterocolitis complicating severe RSV bronchiolitis in PICU settings. Clin Pediatr (Phila). 2024;63(11):1544-1550. Available from: https://doi.org/10.1177/00099228241227763
- Marsicovetere P, Ivatury SJ, White B, Holubar SD. Intestinal intussusception: Etiology, diagnosis, and treatment. Clin Colon Rectal Surg. 2017;30(1):30-39. Available from: https://doi.org/10.1055/s-0036-1593429
- Murdoch Childrens Research Institute. Common viruses trigger most cases of intussusception in children. ScienceDaily. 2024. Available from: www.sciencedaily.com/releases/2024/03/240314122131.htm
- Zheng HT, Zhao QY, Ding Y, Ma SX, Chen WX, Qiu JL, et al. Investigation of the relationships among respiratory syncytial virus infection, T cell immune response, and intestinal flora. Eur Rev Med Pharmacol Sci. 2023;27(6):2671-2678. Available from: https://doi.org/10.26355/eurrev_202303_31804
- Liu J, Huang Y, Liu N, Qiu H, Zhang X, Liu X, et al. The imbalance of pulmonary Th17/Treg cells in BALB/c suckling mice infected with respiratory syncytial virus-mediated intestinal immune damage and gut microbiota changes". Microbiol Spectr. 2024;12(10):e0181224. Available from: https://doi.org/10.1128/spectrum.03283-23
- Surgical Site Infection (SSI) Event: Center for Disease Control. 2010. Available from: http://www.cdc.gov/nhsn/PDFs/pscManual/9pscSSIcurrent.pdf?agree=yes&next=Accept Updated January 2015. Accessed March 3, 2015.
- Andersson CK, Iwasaki J, Cook J, Robinson P, Nagakumar P, Mogren S, et al. Impaired airway epithelial cell wound-healing capacity is associated with airway remodeling following RSV infection in severe preschool wheeze. Allergy. 2020;75(12):3195-3207. Available from: https://doi.org/10.1111/all.14466
- Linfield DT, Gao N, Raduka A, Harford TJ, Piedimonte G, Rezaee F. RSV attenuates epithelial cell restitution by inhibiting actin cytoskeleton-dependent cell migration. Am J Physiol Lung Cell Mol Physiol. 2021;321(1):L189-L203. Available from: https://doi.org/10.1152/ajplung.00118.2021