More Information
Submitted: April 09, 2022 | Approved: May 09, 2022 | Published: May 10, 2022
How to cite this article: Geferso AT, Buta DD, Said AS, Duguma GM. Face mask utilization and associated factors in combating COVID-19 pandemic among government employee in Akaki district administration offices, Oromia, Ethiopia, 2022. J Community Med Health Solut. 2022; 3: 035-047.
DOI: 10.29328/journal.jcmhs.1001018
Copyright License: © 2022 Geferso AT, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Facemask utilization; Associated factors; Government employee; Akaki district
Face mask utilization and associated factors in combating COVID-19 pandemic among government employee in Akaki district administration offices, Oromia, Ethiopia, 2022
Amenti Teka Geferso1* , Derese Desalegn Buta2, Adam Sheikh Said3
, Derese Desalegn Buta2, Adam Sheikh Said3 and Geleta Merga Duguma4
and Geleta Merga Duguma4
1Public Health, Adama General Hospital and Medical College, Ethiopia
2Public Health, University of South Africa, (UNISA), South Africa
3Public Health, Health care and Hygiene, Institute of Medicine, Peoples Friendship University of Russia (RUDN University), Russia
4Reproductive Health, Adama Hospital and Medical College, Ethiopia
*Address for Correspondence: Amenti Teka Geferso, Public Health, Adama General Hospital and Medical College, Ethiopia, Email: [email protected]
Background: The novel coronavirus is a rapidly spreading respiratory disease that has been declared a pandemic by the World Health Organization (WHO) and a global public health emergency. The use of face masks has been recommended by the WHO and the Centers for Disease Control (CDC) as a standard prevention method for transmission of COVID-19.
Objective: The objective of this study is to determine face mask utilization and associated factors in combating the COVID-19 pandemic among government employees in Akaki district administration offices in Akaki District, Oromia, Ethiopia, 2022
Methods: A quantitative cross-sectional study was conducted from December 1, 2021, to February 15, 2022, on 385 government employees working in Akaki district administration offices. After obtaining consent from the study participants, data were collected using pretested, self-administered, and standardized questionnaires adapted from other studies. After the data was collected, it was entered into Epi info version 7.2.6, cleaned, and analyzed using SPSS version 26. A logistic regression model was computed to measure the association between the predictor and outcome variables. A p - value of.05 with a 95% CI was used as the cut-off point to declare the level of statistical significance.
Results: The study showed that the magnitude of good practice for facemask utilization was 213 (53.5%) (95% CI: 1.50, 1.60) for preventing COVID-19. In the multivariate logistic regression analysis, the odds of using face masks among male employees (AOR = 0.275; 95% CI: 0.137, 0.555), employees aged 20-29 (AOR = 0.17; 95% CI: 0.065, 0.481 ), employees aged 30-39 (AOR = 0.260, 95% CI: 0.109, 0.623), employees of less than five family size (AOR = 0.549, 95% CI: 0.303, 0.995), work experience at 6-12 (AOR = 0, 32, 95 CI: 0.120, 0.450), poor knowledge about face mask use (AOR = 0.504, 95% CI: 0.302, 0.844), and employees with a negative attitude (AOR = 0.430, 95% CI: 0.256, 0.721) were factors significantly associated with face mask utilization.
Conclusion: The magnitude of facemask utilization was low (53.5%) compared to other studies. The results of the study showed that age, sex, household family size, work experience, poor knowledge, and the negative attitude of employees toward facemask utilization were among the factors significantly associated with facemask utilization.
Background of the study
The novel coronavirus is a widespread respiratory disease and today a global public health emergency [1]. It is characterized by multiple symptoms, including fever, difficulty breathing, chills, headache, and loss of taste, and it is also severe in older age groups and people with comorbidities [2–4]. Corona virus (COVID-19) was caused by severe acute respiratory syndrome coronavirus (SARS-COV-2) that suddenly appeared in Wuhan, China in December 2019 and spread around the world. It has been declared a pandemic by the WHO and a global public health emergency [5–7].
Ethiopia is one of the developing countries affected by the COVID-19 pandemic and the first case was confirmed on March 13, 2020. The country’s government has taken corrective measures and hygiene measures such as hand washing, physical distancing and staying at home [8].
The population is generally susceptible to this deadly disease, and since there is no effective drug, self-isolation, self-protection, distance, hand washing, sanitizer, and face mask utilization were among the immediate measures to cut the transmission of the COVID-19 virus from person to person [9,10].
Ethiopia is striving to overcome the pandemic and slow the transmission of COVID-19 through mass education, emergency preparedness, contact tracing, isolation and vaccination of high-risk groups to combat the spread of the disease [10].
Among the preventive measures, the use of face masks has been recommended by the WHO and the CDC as the standard prevention method for transmission of COVID-19. It is a medical device designed to cover the mouth, nose and chin that limits the passage of infectious agents by preventing respiratory droplets and splashes from reaching the wearer’s mouth and nose [11,12].
Statement of the problem
COVID-19 is a global health infectious disease that has affected almost all countries and has resulted in thousands of deaths [13]. It has a strong impact and causes higher mortality in people over the age of 60 and those with comorbidities [14]. According to the Ethiopian Institute of Public Health and WHO Africa Region COVID-19 Weekly Bulletin, as of December 12, 2022, there have been a total of 258,152,594 COVID-19 cases and 5,008,204 deaths (CFR = 1.94%) worldwide. In Africa, a total of 6,479,868 confirmed cases and 153,232 deaths were reported across the continent (CFR = 2.4%) and there were 144,898 COVID-19 infections (2.4% of all cases) among health workers in the region. The African continent accounts for 3.4% of global cases and 4.3% of global deaths. Ethiopia reported the highest number of confirmed cases in Africa after South Africa and as of 12 December 2022 the country had recorded a total of 373,115 confirmed COVID-19 cases and 6,829 deaths (4.5%) with a fatality rate of 1.83% [13,14].
During the outbreak of the disease, many countries were unaware and therefore it was not foreseeable. Because of its high rate of transmission, it has presented many challenges to both patients and healthcare professionals who have been fighting it. Since it was declared a global health threat by the WHO on March 11, 2020, it has experienced a health, economic and social crisis. Millions died and were infected by the virus. Now the Omicron variant of COVID-19 is challenging the world and the Omicron variant has been confirmed in more many countries [13,15].
Today the world fears another wave of the Omicron variant of COVID-19, which is highly transmissible and deadly. Although there is a vaccination against COVID-19, the WHO still recommends the use of face masks and other preventive measures to combat the fast-transmitting COVID-19 virus, but studies show that the use rate of face masks in communities and even among health professionals is still very low. According to the systematic meta-analysis on the effectiveness of public health interventions in reducing COVID-19 incidence, transmission and mortality from COVID-19, conducted at Monash University in Melbourne, face mask-wearing was shown to value of 53% contributed to the reduction of COVID-19. 19 incidence, and wearing face masks is considered an effective technique to prevent respiratory infections, including COVID-19, and proper use of face masks by medical workers can reduce contamination from airborne viral respiratory infections decreases by 80% [16–19].
However, studies show that face mask utilization is low. The study, conducted on the practice of wearing masks in the Community in Saudi Arabia, showed that the frequency of wearing face masks in public places, at work or at social gatherings was 87.2%, 80.5%, 80.5%, 47.5% respectively [20].
Studies revealed that facemask utilization is affected by knowledge, attitude, and practice, as well as socio-demographic factors. The study conducted at Wachamo University indicated that knowledge about facemasks was low (29.2%) and knowledge was found to be associated with factors [7].
Another study conducted in the city of Woldia in north-eastern Ethiopia showed that wearing face masks in crowded places was 63.9% and that respondents’ practices regarding face mask use significantly associated with sex, marital status, education and occupation, while the other study was conducted to assess the face mask utilization status of healthcare providers in referral hospitals in the Amhara region, their face mask utilization was shown to be 59.5% [21,22].
Another study conducted among health professionals in the Addis Ababa Police health facilities showed that the face mask usage rate was 33.3% and that the factors associated with the use of face masks were education, profession and knowledge about the use of face masks [23].
Very few studies have been conducted on the proper use of face masks to prevent COVID-19 in the world and in Ethiopia. Most studies were conducted online. However, no studies have been conducted on the status of government employee use of face masks and the factors involved [12].
Therefore, this study aimed to determine the use of face masks and identify associated factors among government employees. It was conducted to identify the gaps and immediate action to address those gaps in relation to employee use of face masks and related factors as it is very important to control the spread of COVID-19 infection. Therefore, the main objective of this study was to determine the use of face masks and associated factors in controlling the COVID-19 pandemic among government employees in Akaki district administration offices, Oromia, Ethiopia.
Significance of study
There are very limited studies in our country concerning facemask utilization among employees. With the growing number of infections and deaths in communities and another wave of the Omicron variant of the COVID-19 outbreak, it is crucial to see facemask utilization and associated factors among government employees to take the necessary steps and measures to protect and help those employees be aware of the pandemic. This study will provide evidence on the facemask utilization of employees working in the Akaki District administration, Oromia Special Zone surrounding Finfinnee, for the concerned bodies that will eventually help them formulate appropriate solutions.
The purpose of this study is to assess facemask utilization and associated factors among employees in Akaki district administration offices in combating COVID-19. In this research, factors associated with facemask utilization was assessed, and conclusions and ways forward were set. Therefore, the findings of the study will be helpful as input to improve the prevention of COVID-19 and improve facemask utilization in the Community as well as among employees based on the recommendations made. Concerned bodies including governments, ministers of health, district health offices, and other government sectors can use the study result to take corrective measures to combat COVID-19 transmission. Stakeholders will take part in the improvement of the prevention of COVID-19. Policymakers will be benefited from the result and recommendation of the study to improve the quality of its implementation.
Study area /setting and period
The study was conducted in Akaki District, which is located in the Oromia Special Zone Surrounding Finfinne in the Oromia Regional State of Ethiopia. Akaki District is located to the east, 47 kilometers away from the capital city, Addis Ababa. The district is bounded on the east by Adea Woreda, on the west by Sebeta Hawas, on the south by Barek Woreda and on the north by Sodo Dachi Woreda. Dukem is the capital of the district. According to the Woreda Health Department, the district has 87,804 inhabitants and 18,293 households. The district has 28 rural kebeles, one city and four health centers, 28 health posts and three private primary clinics in terms of health facilities. This district administration comprises 31 different offices with 630 employees, of whom 397 are male and 233 are female.
Study design and population
In this study, a quantitative institutional-based cross-sectional study design was employed from December 1, 2022, to February 15, 2022. The source population for the study was all government employees currently working in Akaki district administration offices. All employees who were working in randomly selected offices to be interviewed were included in the study. All employees included in the pre-test of the questionnaire and, who were absent due to illness, annual leave was excluded from the study.
Sample size determination and sampling technique
The sample size for the first objective was calculated using a single proportion formula from Akaki District administration employees. With the assumption of 5% Margin of error and 95% CI, Zα/2 = Critical value = 1.96, 10% non-response rate and design effect = 1.5.
The assumption for P, for this study, was 50 % since no similar published research has been conducted in the study area. So, the proportion of facemask utilization was assumed to be 50% based on this:
P (population proportion) = 50% Where n = required Sample size
d = the margin error between the sample and the population = 0.05
The formula for single proportion was applied as follows
Since the total sample size for the study was 384. According to the source from Akaki District administration public service and Human Resource development office, the total employees in the district administration offices (Reference population) were 630 which is < 10,000 population. Design effect (1.5) will be used since we used a two-stage sampling technique (hierarchies), and 10% response rate was considered. Now since the calculated sample size was > 10% of the Population, the correction formula for the finite population was needed to be applied.
Correction Formula for final sample size:
Where: nc = corrected sample size
no = Sample size calculated
N = Population (in this case it is total Households in Akaki District)
nc= (384*630)/1014 =239
The final sample size is corrected to 239
Final sample size (n) = 239*1.5(design effect) = 359
Final sample size (n) = 359+359*10% (response rate) = 395. Therefore, Final sample size for the study was 395 employees.
Sampling procedure and technique
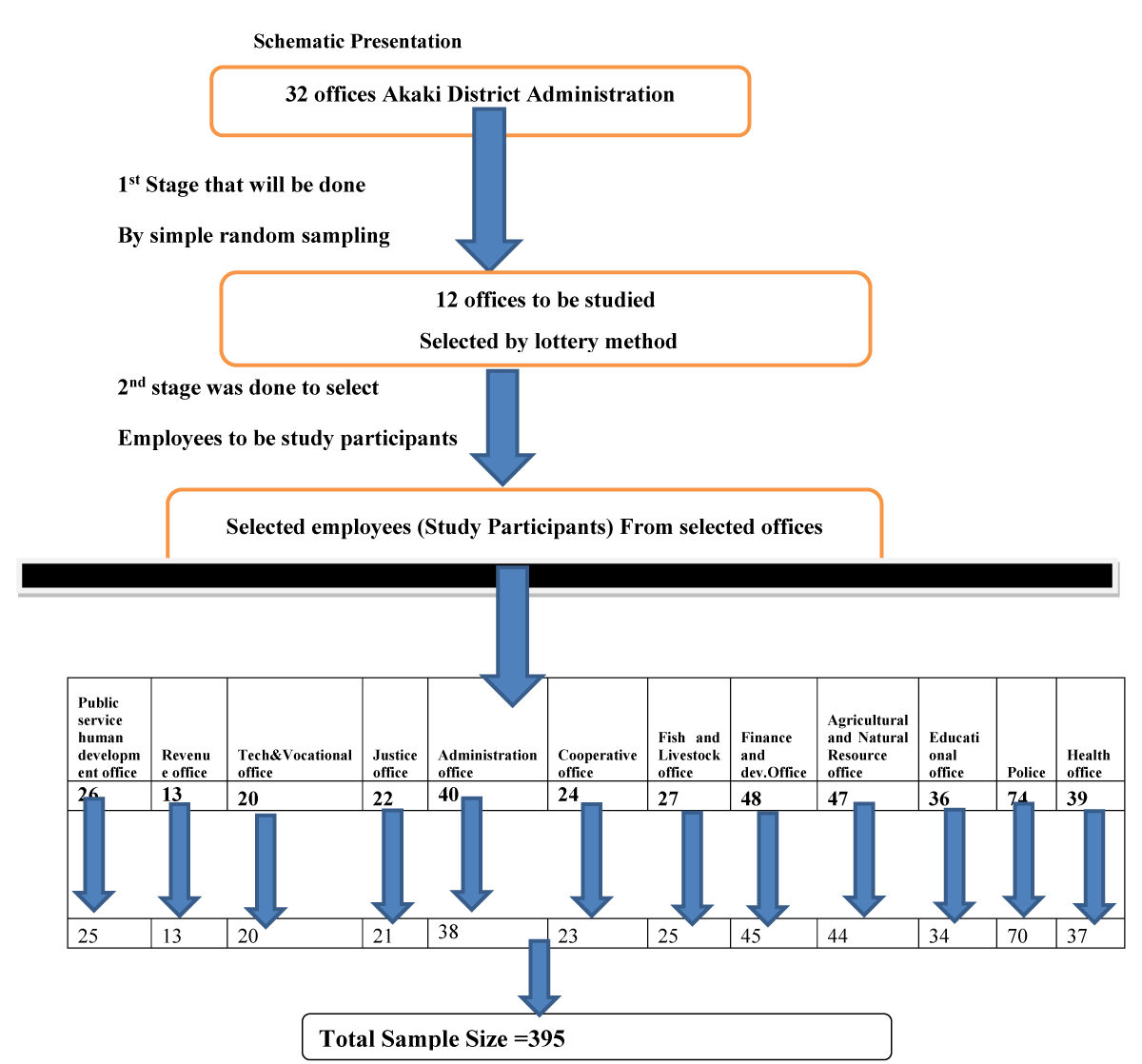
The study was conducted in Akaki district administration offices. In order to obtain study participants, the respondents were selected according to the multi-stage sampling design (two-stage). First, representatives 12 (twelve) offices were selected from the 31 available sectors by simple random sampling (the lottery method was mainly used). The number of employees included in the study was then determined by systematic random sampling in proportion to the total number of employees in the sample base of the selected offices. The calculated sample size using single proportion formula was distributed to selected offices to get the total of study participants from selected offices. The sampling frame (list of all employees) was obtained from the list of daily employee attendance. Employees were selected from offices using systematic random sampling from the list of employees’ attendance available in their offices. The number between one and the sampling interval was first selected using lottery method and the next samples were drawn accordingly (Figure 1).
Figure 1: Schematic presentation for Facemask Utilization and associated factors among employees in Akakki District Administration, Oromia Reagional State, Ethiopia, 2022
Sample for each offices is calculated using ni = n*Ni/N Where ni represents sample for each offices, Ni represents each offices employee (HH), N stands for total employee for selected offices.
Data collection tools and procedures
Data collection tools and procedures: The standardized and structured self-administered questionnaire was developed based on previously available information & published studies. The questionnaire was adapted from published studies with reasonable modifications. The questionnaire was first prepared in English and then translated into Afaan Oromoo language by language experts for data collection and translated back to English for data analysis. It contains variables on socio-demographic, socio-economic characteristics questions, facemask utilization (practices) related questions, factors associated with facemask wearing practices (Knowledge questions, attitude related questions).
Data were collected by three qualified data collectors with BSc degrees in nursing. They were closely monitored under the supervision of the one supervisor and the principal investigator, and were trained by the principal investigator for one day on the aim of the study, how to complete the questionnaire, and maintain privacy and confidentiality during the data collection process.
Data quality assurance: Data quality was maintained using several methods. A standardized questionnaire was first adapted from published studies and prepared with a reasonable modification. The questionnaire was assessed for its validity and reliability and the degree to which items in the questionnaire were relevant and can correctly measure facemask utilization and associated factors and correction was made initially before use. Data collectors and supervisors were given one day training on how to collect, manage, and complete data, as well as interviewing techniques, confidentiality, and how to administer the questionnaire and deal with privacy concerns. Data quality was assured by carefully looking at the relevancy of the questionnaire to the objectives of the study. Before the actual data collection, a pre-test was conducted on 5% of the sample (n = 30) in non-selected nearby offices in the study area (Akaki district administration offices).
The questions were examined for clarity, completeness, and content, and correspondingly adjusted, correctness in terms of content structure, imprecise terminology, ambiguous questions, and language were examined and modified based on feedback obtained during the pre-test.
The internal consistency and reliability were measured using Cronbach’s alpha. Accordingly, the result from Cronbach’s alpha indicated that adequate internal consistency and reliability was 0.82 for Practice of facemask utilization questions and 0.80 for knowledge about facemask utilization questions, and 0.79 attitude of employees toward facemask utilization questions. The data collection process was checked by the principal investigator regularly to ensure that it was complete, accurate, and consistent and that corrective steps were taken.
Data processing and analysis
After the completion of data collection, it was transferred into Epi Info7 version 2.6 and then exported to SPSS version 26 for cleaning and analysis. Finally, descriptive analyses like frequency, percentage, and mean were used to describe the data. A binary logistic regression model was also applied to identify factors associated with community-based health insurance.
Accordingly, those variables with the result of p - value < 0.25 on bivariable logistic regression analysis were considered for multivariable logistic regression analysis. Adjusted Odds Ratio (AOR) with 95% Confidence interval (CI) was used to measure the strength of association and the variable with p - value < 0.05 was taken as statistically significant for multivariable logistic regression analysis.
Operational definitionFace mask: Disposable or re-usable device that creates a physical barrier between the mouth and nose of the wearer and potential contaminants in the immediate environment [24].
Face mask utilization: It is a face mask practice and, in this case, it was expressed by each correct response in the practice category was scored 1 and each incorrect response was zero. The correct response was obtained by summing up items scored and dividing by the total number of items and was above or equal to the mean (average) score it was categorized as Good Practice of facemask utilization and otherwise Poor Practice of facemask utilization [23].
Knowledge about facemask and its utilization: For the convenience of analysis, each correct response in the knowledge category was scored 1 and each incorrect response was entered zero. The correct response was obtained by summing up items scored and dividing by the total number of items and it if was above or equal to the mean (average) score it was categorized under Good Knowledge and otherwise Poor Knowledge [25].
Attitude about face mask use: Respondents were asked attitude related questions to describe their level of agreement to a five Likert scale response format (Strongly disagree to strongly agree) subscale score was obtained by summing up items scored and dividing by the total number of items and if it was above or equal to the mean (average) score it was categorized under Positive attitude and otherwise negative attitudes [7].
Ethical approval
The study ethical approval was received from the Health Research Ethical Review Committee of Oromia Regional Health Bureau before proceeding with actual data collection by the reference number BFO/UBTFU/1-16/4654. The Health Research Ethical Review Committee wrote the letter of approval to the Oromia Special Zone surrounding Finfinnee Health Bureau and the formal letter was written to the Akaki District Administration Health Office. Then the letter of support was written from the Akaki District Health office to each selected offices in Akaki District administration. Respondents were given detailed information about intent, potential benefits and side effects, the right to continue or withdraw from the interview, and the aim of the study, and were given consent to read it for those who could, and the interviewers read it for those who couldn’t. Each respondent was informed that their data would be treated confidentially. Respondents had complete freedom to withdraw from the study or refuse to complete questionnaires at any time.
Socio-demographic & economic characteristics of the respondents
A total of 385 employees participated in the study with a 97.5% response rate and more than half of the respondents. Two hundred fifty seven (68.8%) were men and one-third, 128(33.2%), were female. The mean and standard deviation of the age of the study participants were 31.23 ± 5.093, respectively. Oromo ethnic group was the largest in the study area which accounts for 365(94.8%) of the study participants. The religious status of the study participants showed that half of the study participants 196(50.9%) were Orthodox and 121(31.4%), 56(14.5%), and 12(3.1%) were Protestant, Waaqeffataa, and Muslim respectively. The study indicated that more than half of the respondents, 229(59.5%) were degree holders and 146(37.9%), 8(2.1%), 2(0.5%) were diploma, less than or equal to 10th grade, and masters’ holders respectively. The marital status of the respondents showed that 229(59.5%) of the study participants were married and 156(40.5%) were unmarried. Two hundred twenty nine (59.5%) of the respondents had more than five (> 5) family members, and 156(40.5%) had less than or equal to five family members. The mean and standard deviation of household family size of the respondents was 3.12 ± 1.84, respectively. The study showed that 302 employees (78.4%) recorded a monthly income of more than five thousand Ethiopian Birr (5,000 ETB), and the mean annual income of the participants was 5713.42 ETB with an SD of 1338.722 (Table 1).
Facemask utilization status
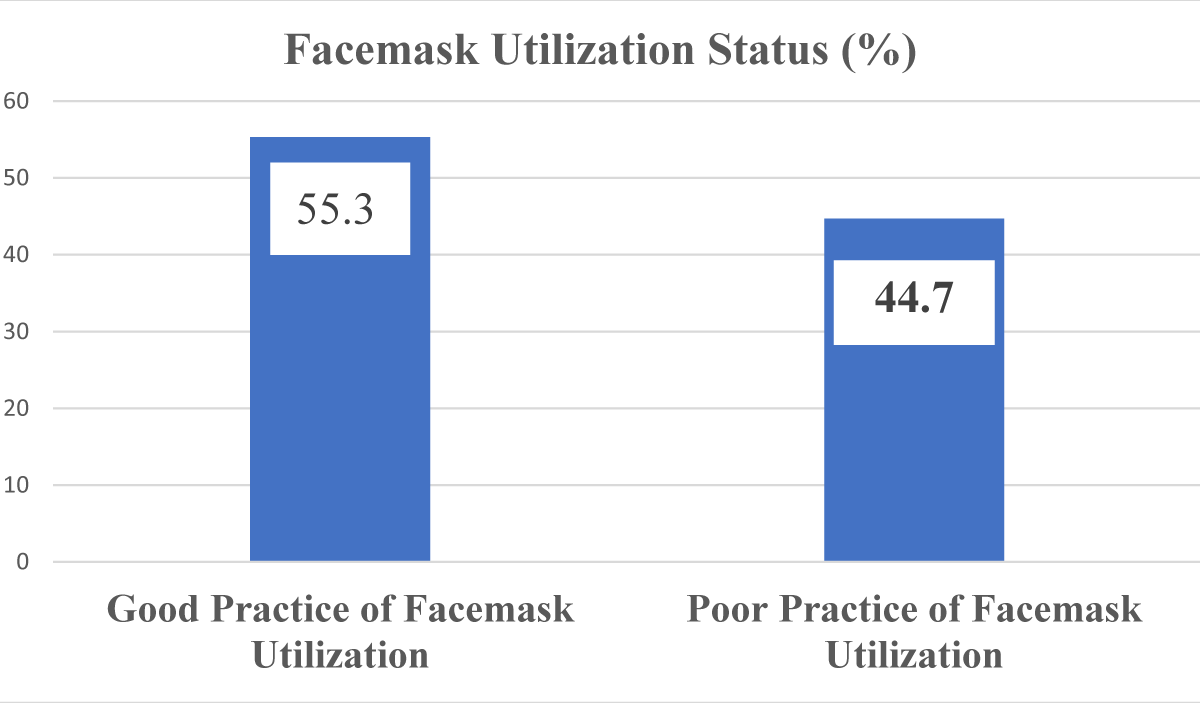
The study found that 213 (53.5%) (95% CI: 1.50-1.60) of the 385 respondents had a good practice of facemask utilization to prevent COVID-19 (Figure 2).
Figure 2: Facemask Utilization status among Akaki District administration employees, 2022.
| Table 1: Socio-demographic & economic Characteristics of Respondents, Akaki District administration employee, 2022 | |||
| Attributes | Categories | Frequency | Percent (%) |
| Sex | Male | 257 | 68.8 |
| Female | 128 | 33.2 | |
| Age | 20-29 | 101 | 26.2 |
| 30-49 | 229 | 59.5 | |
| ≥ 40 | 55 | 14.3 | |
| Ethnic group | Oromo | 365 | 98.4 |
| Amhara | 20 | 5.2 | |
| Religion | Orthodox | 196 | 50.9 |
| Muslim | 12 | 3.1 | |
| Waaqeffataa | 56 | 14.5 | |
| Protestant | 121 | 31.4 | |
| Educational status | ≤ 10th Grade | 8 | 2.1 |
| Diploma | 146 | 37.9 | |
| Degree | 229 | 59.5 | |
| Masters | 2 | 0.5 | |
| Marital status | Single | 156 | 40.5 |
| Married | 229 | 59.5 | |
| Household members (Family Size) | ≤ 5 | 156 | 40.5 |
| > 5 | 229 | 59.5 | |
| Monthly income | < 5000 | 83 | 21.6 |
| ≥ 5000 | 302 | 78.4 | |
Thirteen practice related questions were used to assess the status of facemask utilization among Akaki District administration employees. Based on the responses to the questions, the practices of respondents toward wearing a facemask in public places to protect themselves against COVID-19 were assessed and 341 (88.6%) of them responded that they do so, while the rest responded that they didn’t. The study found that more than two-thirds of respondents (300, or 77.9%) do not remove their facemask when they want to speak, while 85(22.7%, remove their facemask while talking.
Even though the surgical mask is disposed of after use, 216(56%) of respondents claimed that they do not store the used surgical mask in a bag or pocket for later use while 169(43.9%) said they store the facemask for later use. It is recommended to clean hands before and after wearing a mask.
However, respondents were asked if they clean their hands before and after wearing masks. Of these, 297(77.1%) responded that they clean their hands before and after wearing a mask, while their peers did not.
On the other hand, respondents were asked whether they confirmed the metal noseband on the top and wear it and 305(79.2%) reported that they confirmed the availability of the metal noseband on the top of their mask while 80(20.8%) of respondents didn’t confirm it. Subsequently, 272(70.6%) touch the mask they once wore and 113(29.4%) do not touch the mask they once wore. In this study, 325(84.4%) of the respondents identified the outer and inside parts of the mask, while 60(15.6%) responded that they did not. The facemask should not be worn for more than 8 hours, but this study identified that 279(59.5%) wear the facemask repeatedly and the rest did not. Regarding the point of starting to wear a face mask, the respondents were asked and responded that 228(59.5%) started wearing their mask from their home and 93(24.2%), 64(16.6%) started wearing masks starting from entry of transportation, at workplace/office, respectively (Table 2).
| Table 2: Practice of Facemask Utilization status, Akaki District administration employees, 2022. | ||||
| S,N | Variables | Category | Frequency | Percent (%) |
| 1 | Wear facemask at public places to protect against facemask | Yes(correct) | 341 | 88.6 |
| No | 44 | 11.4 | ||
| 2 | Remove facemask when want to speak | Yes | 85 | 22.1 |
| No(correct) | 300 | 77.9 | ||
| 3 | Store the used surgical mask in a bag or pocket for a later use | Yes | 169 | 43.9 |
| No (correct) | 216 | 56.1 | ||
| 4 | Clean hands before and after wearing a mask | Yes(correct) | 297 | 77.1 |
| No | 88 | 22.9 | ||
| 5 | Do Confirm the metal noseband on the top and wear it? | Yes (Correct) | 305 | 79.2 |
| No | 80 | 20.8 | ||
| 6 | Do you Touch the facemask once wore | Yes | 272 | 70.6 |
| No(correct) | 113 | 29.4 | ||
| 7 | Identify the inside and outside parts of the facemask before wearing | Yes(correct) | 325 | 84.4 |
| No | 60 | 15.6 | ||
| 8 | Use single mask repeatedly | Yes | 229 | 59.5 |
| No(correct) | 156 | 40.5 | ||
| 9 | Eat/smoke/drink during mask-wearing | Yes | 349 | 90.6 |
| No (Correct) | 36 | 9.4 | ||
| 10 | From where do you start mask-wearing? | Starting from Home | 228 | 59.2 |
| Starting from the entry of transportation | 93 | 24.2 | ||
| At workplace/office | 64 | 16.6 | ||
| 11 | Always wear facemask at working place/office | Yes(correct) | 261 | 67.8 |
| No | 124 | 32.2 | ||
| 12 | Dispose the mask when wet or soiled | Yes(correct) | 300 | 77.9 |
| No | 85 | 22.1 | ||
| 13 | Do you extend the facemask to cover the nose, mouth, and chin? | Yes (correct) | 333 | 86.5 |
| No | 52 | 13.5 | ||
| The overall practice of facemask utilization | The poor practice of facemask utilization | 172 | 44.70% | |
| Good practice of facemask utilization | 213 | 55.30% | ||
Knowledge of Akaki district employees toward facemask utilization
Nine (9) knowledge related questions were used to measure the respondents’ knowledge level about the facemasks utilization. Respondents’ overall knowledge of facemask utilization was classified as good for those who answered above the mean score and poor for those who answered below or equal to the mean score. According to the findings, 229(59.5%) of all respondents had good knowledge of facemask utilization, whereas 156(40.5%) had poor knowledge (Table 3).
Respondents were asked to rate their understanding of how to use surgical facemasks to protect against COVID-19. Based on this three hundred thirty seven (87.5%) said the white side of the facemask should face in, while 48(12.5%) said the white side should face out. When asked about the number of layers in the facemask, 168(43.6%), 152(39.5%), and 65(16.9%) said there were two, three, and four layers, respectively (Table 3).
| Table 3: Knowledge about facemask utilization of Akaki District administration employees, 2022. | |||
| Variables | Category | Frequency | Percent (%) |
| Which is the correct way of using a surgical face mask to protect against COVID-19? | The white side facing out | 48 | 12.5 |
| The white side facing in (Correct) | 337 | 87.5 | |
| How many layers are there in a surgical mask? | Two | 168 | 43.6 |
| Three | 152 | 39.5 | |
| Four | 65 | 16.9 | |
| Can wearing a surgical mask protect you from COVID-19? | Yes | 305 | 79.2 |
| No | 80 | 20.8 | |
| Which layer acts as a filter media barrier | First Layer | 232 | 60.3 |
| Middle Layer | 153 | 39.7 | |
| Which type of masks protect against COVID-19 | 95% BFE and PFE | 160 | 41.6 |
| 97% BFE and PFE | 44 | 11.4 | |
| 99% BFE and PFE | 181 | 47 | |
| How long can you wear a surgical mask | 4 hours | 165 | 42.9 |
| 8 hours | 220 | 57.1 | |
| For proper wearing, to which extent the surgical mask should cover? | Nose only | 60 | 15.6 |
| Nose and mouth | 80 | 20.8 | |
| Nose, mouth, and chin | 245 | 63.6 | |
| What is the purpose of the metal strip on a surgical mask | No purpose | 60 | 15.6 |
| To fit on the nose | 285 | 74 | |
| To fit on the chin | 40 | 10.4 | |
| Is the cloth facial mask as effective as a regular surgical facial mask | Yes | 212 | 55.1 |
| No | 173 | 44.9 | |
| Overall Knowledge Score of Employees toward facemask utilization | Poor Knowledge of Employees toward facemask utilization | 156 | 40.5 |
| Good Knowledge of Employees toward facemask utilization | 229 | 59.5 | |
Respondents were, on the other hand, asked to rate how well they understood which layer functions as a filter media. Only 153 people (39.7%) were aware that the middle layer serves as filter media, while 232 people (60.3%) were aware that the first layer serves as filter media. When asked which type of facemasks are used to defend against COVID-19, 16(41.6%) responded 95% BFE and Personal protective equipment (PPE) facemasks type, 44(11.4%) said 97% BFE and PFE facemasks type, and 181(47%) said 99% BFE and PFE facemasks type, respectively (Table 3).
When respondents asked for how long facemasks should be worn, 220(57.1%) said the facemask should be worn for 8 hours, while 165(42.9%) said it should be worn for 4 hours. When asked which part of the face a facemask should cover, 245(63.6%) said it should cover the nose, mouth, and chin, while the others said it should cover the nose, mouth, and chin, and 60(15.6%) said it should cover the nose and mouth. Following that, respondents were asked for their thoughts on whether a cloth facemask is as effective as a standard surgical facemask, and 212(55.1%) said agreed that it is as effective as a surgical face mask, while 173(44.9%) said no (Table 3).
The attitude of employees toward facemask utilization
Employee attitudes were measured using eight (8) five-point Likert scale items (strongly disagree, disagree, neutral, agree, and strongly agree) that were coded one (1) to five (5). The mean score was determined, and those who answered below or equal to the mean score were classified as having a negative attitude, while those who answered above the mean score were classified as having a positive attitude (Table 4).
| Table 4: Attitudes of Akaki District administration employees toward facemask utilization, 2022. | ||||||||||
| Variables | Strongly disagree | Disagree | Neutral | Agree | Strongly agree | |||||
| N | % | N | % | N | % | N | % | N | % | |
| Do you think that facemask needs to be carefully put on and taken off? | 40 | 10.4 | 64 | 16.6 | 8 | 2.1 | 136 | 35.3 | 137 | 35.6 |
| do you store the used surgical mask in a bag or pocket for later use | 64 | 16.6 | 152 | 39.5 | 24 | 6.2 | 124 | 32.2 | 21 | 5.5 |
| Do you clean your hands before and after wearing masks? | 16 | 4.2 | 85 | 22.1 | 28 | 7.3 | 124 | 32.2 | 132 | 34.3 |
| Do you agree that wearing face mask prevents covid-19 transmission | 24 | 6.2 | 80 | 20.8 | 12 | 3.1 | 149 | 38.7 | 120 | 31.2 |
| Do you agree that it is difficult to communicate with a facemask? | 28 | 7.3 | 148 | 38.4 | 28 | 7.3 | 101 | 26.2 | 80 | 20.8 |
| Do you think that a face mask should cover the mouth, nose, and chin? | 32 | 8.3 | 72 | 18.7 | 16 | 4.2 | 105 | 27.3 | 160 | 41.6 |
| Do you agree that appropriate size of mask is important to wear | 24 | 6.2 | 88 | 22.9 | 12 | 3.1 | 125 | 32.5 | 136 | 35.3 |
| Do you think that it is necessary to wear a face mask as you are afraid of getting COVID-19? | 32 | 8.3 | 88 | 22.9 | 8 | 2.1 | 125 | 32.5 | 132 | 34.3 |
| Attitude Score of Employees toward facemask utilization | Negative Attitude of Employees toward facemask utilization | 136 | 35.3 | |||||||
| Positive Attitude of Employees toward facemask utilization | 249 | 64.7 | ||||||||
Following the procedure, the study found that 249 people (64.7%) had a positive attitude toward facemask use, while 136 people (35.3%) had a negative view. When asked if facemasks should be carefully put on and removed, 40(10.4%) disagreed, while 137(35.6%) strongly agreed. When asked whether wearing a facemask helps prevent COVID-19 transmission, 31.2%(120) strongly agreed, 149(38.7%) agreed, and 24(6.2%) disagreed (Table 4).
Factors associated with the practice of facemask utilization
Bivariate logistic regression and multivariable analysis were carried out to determine independent predictors of facemask utilization. Those candidate variables with a p - value < 0.25 in bivariate logistic regression were included in the multivariable logistic regression model and considered significant in the model at a p - value less than 0.05.
A result of bivariate logistic regression applied to identify significant independent variables showed that facemask utilization was significantly associated (p < 0.25) with the sex, ethnic group, religion, age, household family size, monthly income, work experience, knowledge, and attitude of employees toward facemask utilization were significantly associated with facemask utilization. However, in the multivariate logistic regression analysis, sex, religion, age, household family size, work experience, knowledge, and attitude of employees were found to be significantly associated with facemask utilization (Table 5).
| Table 5: Multivariate analysis of Factors Associated with facemask utilization among employees in Akaki district administration offices, 2022. | ||||||
| Variables | Category | Facemask Utilization Status | COR (95% CI) | AOR (95%CI) | p - value | |
| Poor facemask utilization | Good facemask Utilization | |||||
| Sex | Male (1) | 135(52.5%) | 122(47.5%) | 0.367(0.233,0.578) | 0.275(0.137,0.555) | 0 |
| Female (2) | 37(28.9%) | 91(71.1%) | ||||
| Religion of Respondents | Orthodox | 90(45.9%) | 106(54.1%) | |||
| Muslim | 10(83.3%) | 2(16.7%) | 0.172(0.36,0.820) | |||
| Waaqeffataa | 16(28.6%) | 40(71.4%) | 2.154(1.090,4.256) | 2.536(1.113,5.778) | 0.05 | |
| Protestant | 56(46.3%) | 65(53.7%) | Ref | |||
| Age of Respondents | 20-29 | 52(51.5%) | 49(48.5%) | 0.322(0.156,0.662) | 0.117(0.065,0.481) | 0.001 |
| 30-39 | 106(46.3%) | 123(53.7%) | 0.396(0.205,0.767) | 0.260(0.109,0.623) | 0.003 | |
| > = 40 | 14(25.5%) | 41(74.5%) | Ref | |||
| Household Size | ≤ 5 | 82(52.6%) | 74(47.4%) | 0.584(0.387,0.882) | 0.549(0.303,0.995) | 0.048 |
| > 5 | 90(39.3%) | 139(60.7%) | Ref | |||
| Work Experience | < 6 years | 19(27.5%) | 50(72.5%) | |||
| 6-12 years | 132(62.3%) | 80(37.7%) | 0.153(0.088,0.267) | 0.232(0.120,0.450) | 0.000 | |
| 12-28 years | 21(20.2%) | 83(79.8%) | ||||
| knowledge about facemask utilization | Poor knowledge about facemask utilization | 96(61.5%) | 60(38.5%) | 0.310(0.203,0.474) | 0.504(0.302,0.844) | 0.009 |
| Good knowledge about facemask utilization | 76(33.2%) | 153(66.8%) | ||||
| Attitude toward facemask utilization | Negative attitude toward facemask utilization | 76(55.9%) | 60(44.1%) | 0.495(0.324,0.757) | 0.430(0.256,0.721) | 0.001 |
| Positive attitude toward facemask utilization | 96(38.6%) | 153(61.4%) | ||||
The study revealed that male employees were less likely to use facemask (AOR = 0.275; 95% CI: 0.137, 0.555) compared to female employees. The odds of facemask Utilization for Waaqeffata religion followers were 2.56 times (AOR = 2.56; 95% CI: 1.113, 5.778) higher compared to other religious groups. Employees within the age of 20-29 (AOR = 0.117, 95% CI: 0.065, 0.481) and age between 30-39 (AOR = 0.260, 95% CI: 0.109, 0.623) were found to be less likely to use facemask compared to those employees within the age range ≥ 40 years (Table 5).
In this study, facemask utilization was also found to be associated with employees’ family size. Employees with ≤ 5 family size were 45% less (AOR = 0.549, 95% CI: 0.303, 0.995) likely to utilize facemask compared to those employees with > 5 household family size. In this study, Work experience was also found to be a significantly associated factor. The odds of facemask utilization among employees with 6-12 years of work experience were found to be 76.8% less (AOR = 0.232, 95% CI: 0.120, 0.450) compared to those employees who worked for 12-28 years (Table 5).
Employee knowledge about facemask utilization, on the other hand, was found to be strongly associated with facemask utilization. Employees with poor knowledge of facemask utilization had 49.6% less likely of using facemask (AOR = 0.504, 95% CI: 0.302, 0.844) than those with good knowledge (Table 6). Similarly, the study showed that the odds of facemask utilization among those employees with negative attitudes toward facemask utilization was found to be 57% less (AOR = 0.430, 95% CI: 0.256, 0.721) compared to those employees with a positive attitude toward facemask utilization (Table 5).
This study found that the magnitude of facemask utilization among Akaki District government employees was 55.3% (95% CI: 1.50 - 1.60). This finding was lower than the findings of studies conducted in Saudi Arabia (87.2%), Bangladesh (89%), Pakistan (75%), India (67%), among university students in Vietnam (76.5%), in metropolitan towns of the Amhara region (57.1%), in Amhara region referral hospitals (59.5%), Woldia town (63.9%), Dassie health center (69.3%). However, the current study is higher compared to the studies conducted in Malaysia which were (51.2%), Pakistan (35.2%), in Addis Zemen Hospital (36.6%), in a police health facility in Addis Ababa (33.3%), and almost similar to the study conducted in Dassie and kombolcha among taxi drivers which were (54.68%). The disparities could have resulted from the difference in awareness creation activities done by media, government bodies, health professionals, influential persons and might be due sociocultural factors, time difference, the background of study participants, and study setting [5,6,11,22,24,26-33].
This study identified that male employees were 72.5% less likely to use facemask (AOR = 0.275; 95% CI: 0.137, 0.555) compared to female employees. This finding was contrary to the observational study conducted in South Asian countries where facemask utilization was found to be 1.28 times higher among females compared to male individuals [33] and the study conducted among university students in Vietnam where facemask utilization among the male gender was 1.5 times higher compared to females [6], This finding was also inconsistent with the study conducted in Tigray which showed that males were two times more likely to wear a mask than females [34]. Differences in findings could have resulted from the time difference, study setting, and study population.
Another factor associated with mask use in this study was religion. This study found that the use of face masks by people of the Waqeffata religion followers was 2.536 times higher (AOR = 2.536; 95% CI: 1.113, 5.778) compared to other religious groups. This finding is inconsistent with an observational study carried out in a South Asian country where Muslims were 6.19 times more likely to wear a mask than non-Muslims. Discrepancies could have arisen from differences in beliefs, differences in religious doctrines, and differences in the efforts of religious leaders to raise awareness [33].
Facemask utilization, on the other hand, was found to be associated with the age of employees. Employees in the age range of 20-29 were 88.3% less likely to use a facemask (AOR = 0.117, 95% CI: 0.065, 0.481) and employees in the age range of 30-39 were 74% less likely to use a facemask (AOR = 0.260; 95% CI: 0.109, 0.623) compared to those in the age range of 12-28 years. This finding appears to contradict a study conducted in Tigray, which found that facemask use was twelve times greater among those over 50 years old and 2.5 times higher among those aged 18-29 years old. The findings’ inconsistency could be related to differences in socio-economic backgrounds, study populations, and study areas, as well as a lack of facemask use among young people (12-28 years) and fear of COVID-19 among older people due to its high death rate among the elderly (> = 50 years) [34].
Unlike other studies, the household family size was revealed to be an associated factor in this one. Employees with a household size of less than or equal to five family members were 45.1% less likely to use a facemask (AOR = 0.549, 95% CI: 0.303, 0.995) than those with a household size of more than five. This could be because as the number of families increases, employees’ feelings of responsibility increase as well.
Employee work experience was also discovered to be a factor influencing the use of facemasks. Employees with six to twelve years of work experience were less likely to use a facemask (AOR = 0.504, 95% CI: 0.302, 0.844), according to the study, than those with 12 to 28 years of work experience. This finding is nearly similar to that of a study conducted in Northwest Ethiopia, which found that health care personnel with 6-10 years of experience were 2.22 times more likely than those with eleven or more years of experience to have poor COVID-19 preventive practice. This might be because as individuals’ work experience grows, so does their exposure to and dread of such epidemics. Another cause could be a difference in occupation, study design, study population, work environment, and enforcement of wearing a facemask at work from government offices [35].
According to this study, knowledge about the facemask utilization of employees was found to be the factor associated with proper facemask utilization. As to this study, the overall knowledge score of facemask utilization about facemask utilization was reported 229(59.5%). This finding is extremely lower compared to the study conducted in Malaysia (80.5%), among university students in Vietnam (89.7%), Lower compared to the study conducted in Saudi Arabi (86.6%), Pakistan (73%), Amhara region metropolitan cities (76%), Amhara region referral hospitals (65.8%) [6,22,26,36,37]. This disparity could be attributed to differences in health coverage, disparities in COVID19 awareness, disparities in awareness creation strategies among study areas (countries), and differences in sociocultural and economic levels.
Employees with poor knowledge of facemask utilization were reported to be less likely to use facemask (AOR = 0.504, 95% CI: 0.302, 0.844) than those with good knowledge of facemask use, according to the study. This finding is consistent with a study of health care workers in Addis Ababa Police health facilities, which found that those with poor knowledge of facemask use were less likely to use it properly than those with good knowledge [23]. However, it is contrary to a study conducted in metropolitan towns of the Amhara region, Ethiopia where the odds of good facemask wearing practice of respondents who had good knowledge were about three times higher than those who had poor knowledge was reported [38]. The discrepancies in the findings could have been caused by differences in employee understanding of the severity of the COVID-19 pandemic; the more employees recognized the severity of the epidemic, the more they dreaded it and used facemasks to protect themselves. Differences in professional status, educational level, access to information, advocacy and study design, and socio-demographic characteristics could all be issues.
This finding, on the other hand, contradicted a study conducted with quarantined adults in the Tigrai region, which found that those who knew about facemasks were two times more likely to use facemask than those who didn’t [39]. This disparity could be attributable to differences in COVID-19 exposure, as individuals who were in quarantine had had more exposure to the disease and are more familiar with preventive measures. Other considerations include differences in study design, living circumstances, and socio-economic factors.
Furthermore, this result contradicts another study conducted in Addis Zemen Hospital, Amhara region, Ethiopia, which found that patients with inadequate knowledge of COVID-19 were 8.6 times more likely to have poor practice, which included wearing facemasks [40]. This could be the result that facemask utilization goes with knowing how to use a facemask and its benefits.
The study participants’ attitude toward facemask use was another factor discovered as a predictor factor associated with facemask utilization. This study found that 249(64.7%) had a good attitude toward facemask utilization, which is nearly similar to the findings of a study conducted in Dassie and kombolcha towns (67.6%) and a study conducted in Amhara region metropolitan towns (68.3%), Lower than the study conducted among Vietnamese university students (72.8%) and lower than the study conducted in Malaysia (83.1%), but greater than the study conducted in the Addis Ababa police hospital (45.3%) [6,11,26,30,41]. To properly implement face mask-wearing requirements, more information is needed, as well as a positive attitude and the absence of misunderstandings about information. This encourages a positive outlook, which can aid in the reduction of misunderstandings and the promotion of best practices.
This finding showed that the odds of good facemask utilization among those government employees who had a negative attitude toward facemask utilization was 57% less (AOR = 0.430, 95% CI: 0.256, 0.721) compared to those employees who had a positive attitude toward facemask utilization. This study is consistent with the study conducted in Vietnam where attitude had an association with facemask use [6]. This could be because the mindset includes everything. This finding contrasted with another study conducted in the Amhara region, Northwest Ethiopia, which found that communities with a good attitude were 2.279 times more likely to use masks than communities with a negative attitude [38]. These discrepancies could have resulted from the fact that a person’s perspective and attitude are driving forces in their ability to do any activity, revealing that attitude is important in disease prevention.
When compared to prior studies, the magnitude of proper facemask utilization in the study area was low (55.3%). The study’s findings revealed that age, sex, household family size, employee religion, employee work experience, knowledge of facemask utilization, and attitude toward facemask utilization were all significantly associated with proper facemask utilization. Concerned bodies should work hard to improve COVID-19 prevention measures by enhancing facemask use in the workplace, public spaces, and crowds, and should strictly regulate.
As a result, the woreda health office and concerned officials, Woreda administrative offices, health professionals, and stakeholders should work hard to disseminate information on the utilization of facemasks and raise employee awareness and work to change the attitude of employees. They should also take corrective action to improve COVID-19 prevention measures. Facemask use in the workplace, public spaces, and crowds should be strictly regulated by the government.
Recommendation
i). To all Levels of district, zonal Health, Regional Offices and Federal Ministry of Health
They should provide employees with training on facemask wearing and the benefits of facemask use, as well as continue to strengthen information and communications activities, enhance behavioral change activities to raise employee awareness so that facemask utilization can be improved, attitude and behavioral change can be achieved and finally the pandemic could be overcome
ii). To all levels of district administration sectors, Leaders and stake holders
All levels of district administration sectors, leaders, and stakeholders should work more to increase the use of facemasks among government employees at the workplace and ensure the availability of COVID-19 preventive supplies, enhance the regulation as well as managers/leaders should be committed to motivating staff to use facemasks more frequently.
iii) To all employees in the district administration offices
Employees should participate in the establishment of awareness, attend training, expand their understanding of facemask use, and urge their families and friends to use facemasks appropriately to combat COVID-19.
iV) To all health Professionals
Health professionals should be committed to work hard in providing, training, follow-up, supporting other employees to use facemask to prevent themselves from COVID-19.
V) To Researchers and scholars
Researchers should concentrate on the factors that are associated with the utilization of facemasks in the prevention of COVID-19, and further study should be conducted to learn more about the factors that are linked to the use of facemasks in the prevention of COVID-19
Data availability: The data used to support the findings of this study are available and can be accessed from the primary author on reasonable request.
Additional points
Strength of the study: This research can help district health offices and other sectors focus on facemask use and associated issues. Because the information was gathered from employees, it aids in the improvement of COVID-19 prevention strategies. The data were gathered from educated government personnel who freely filled out a self-administered questionnaire. The data collection and data input were strictly supervised, and the analysis and cleaning were meticulously completed using the latest versions of computer applications, Epi info7 version 7.2.6 and SPSS version 26.
Limitation of the study: The study aimed to assess all aspects associated with facemask use, but it was not exhaustive, and other factors may exist that were not discovered in this study. Some associated factors, such as employee family size, were impossible to compare to other studies due to a lack of similar studies. The study’s other drawback is that there weren’t enough comparable studies in Ethiopia and the study area to utilize as a literature review, and due to this, making comparisons was too difficult. Some of the research was done online and was not the same as the research that was done in person. The COVID-19 pandemic by itself hampered to conduct of free contact and interview with respondents and due to this, it was not possible to add more qualitative information to the study.
Conflicts of the interest: The authors declare no conflict of interest in this research work .
Author contribution: The authors significantly contributed to the work of this study and the correspondent took part in drafting revising /reviewing it. The agreement was made with the journal to which the article has been sent for publication.
I am grateful to the Akaki District Health office for prompting me to prepare this research. My gratitude goes to the Oromia Health Bureau for providing the ethical approval. I am also grateful and honored to my advisors Dr. Derese Desalegn Buta (BSc, MPH and Ph.D.) to express my special thanks and deep appreciation for effectively guiding and encouraging me to write this research paper. My gratitude goes to Dr.Adam Sheikh Said (MD, Ph.D.), and Mr Geleta Merga Duguma(MPH) for their courageous support in writing up of the research. My special thanks go to the Public Service and Human Resources Development Office of Akaki District Administration who kindly provided me with information about employees in the district and I do not hesitate to thank all my data collectors, supervisors, families and associates.
Funding: No funded raised from institutions or other sources and the study was conducted by the researcher.
- Yazew BG, Abate HK, Mekonnen CK. Knowledge, Attitude and Practice Towards COVID-19 in Ethiopia: A Systematic Review; 2020. Patient Prefer Adherence. 2021 Feb 15;15:337-348. doi: 10.2147/PPA.S288186. PMID: 33623375; PMCID: PMC7894797.
- Saadatjoo S, Miri M, Hassanipour S, Ameri H, Arab-Zozani M. Knowledge, attitudes, and practices of the general population about Coronavirus disease 2019 (COVID-19): a systematic review and meta-analysis with policy recommendations. Public Health [Internet]. 2021;194:185–95. https://doi.org/10.1016/j.puhe.2021.03.005
- Bekele D, Tolossa T, Tsegaye R, Teshome W. The knowledge and practice towards COVID-19 pandemic prevention among residents of Ethiopia. An online cross-sectional study. PLoS One. 2021 Jan 28;16(1):e0234585. doi: 10.1371/journal.pone.0234585. PMID: 33507906; PMCID: PMC7843015.
- Tesfaye ZT, Yismaw MB, Negash Z, Ayele AG. COVID-19-Related Knowledge, Attitude and Practice Among Hospital and Community Pharmacists in Addis Ababa, Ethiopia. Integr Pharm Res Pract. 2020 Aug 24;9:105-112. doi: 10.2147/IPRP.S261275. PMID: 32904494; PMCID: PMC7455591.
- Fikadu Y, Yeshaneh A, Melis T, Mesele M, Anmut W, Argaw M. COVID-19 Preventive Measure Practices and Knowledge of Pregnant Women in Guraghe Zone Hospitals. Int J Womens Health. 2021 Jan 7;13:39-50. doi: 10.2147/IJWH.S291507. PMID: 33442303; PMCID: PMC7800450.
- Duong MC, Nguyen HT, Duong BT. A Cross-Sectional Study of Knowledge, Attitude, and Practice Towards Face Mask Use Amid the COVID-19 Pandemic Amongst University Students in Vietnam. J Community Health [Internet]. 2021;(0123456789). https://doi.org/10.1007/s10900-021-00981-6
- Larebo YM, Abame DE. Knowledge, attitudes, and practices of face mask utilization and associated factors in COVID-19 pandemic among Wachemo University Students, Southern Ethiopia: A cross-sectional study. PLoS One. 2021 Sep 20;16(9):e0257609. doi: 10.1371/journal.pone.0257609. PMID: 34543358; PMCID: PMC8451998.
- Shiferie F. Improper disposal of face masks during COVID-19: unheeded public health threat. Pan Afr Med J. 2021 Apr 14;38:366. doi: 10.11604/pamj.2021.38.366.29063. PMID: 34367445; PMCID: PMC8308934.
- Ma L, Liu H, Tao Z, Jiang N, Wang S, Jiang X. Knowledge, Beliefs/Attitudes, and Practices of Rural Residents in the Prevention and Control of COVID-19: An Online Questionnaire Survey. Am J Trop Med Hyg. 2020 Dec;103(6):2357-2367. doi: 10.4269/ajtmh.20-0314. Epub 2020 Oct 27. PMID: 33124537; PMCID: PMC7695081.
- Defar A, Molla G, Abdella S, Tessema M, Ahmed M, Tadele A, Getachew F, Hailegiorgis B, Tigabu E, Ababor S, Bizuwork K, Deressa A, Tasaw G, Kebede A, Melese D, Gashu A, Eshetu K, Tayachew A, Wossen M, Hassen A, Habebe S, Assefa Z, Abayneh A, Abate E, Tollera G. Knowledge, practice and associated factors towards the prevention of COVID-19 among high-risk groups: A cross-sectional study in Addis Ababa, Ethiopia. PLoS One. 2021 Mar 11;16(3):e0248420. doi: 10.1371/journal.pone.0248420. PMID: 33705480; PMCID: PMC7951807.
- Tadesse T, Tesfaye T, Alemu T, Haileselassie W. Healthcare Worker's Knowledge, Attitude, and Practice of Proper Face Mask Utilization, and Associated Factors in Police Health Facilities of Addis Ababa, Ethiopia. J Multidiscip Healthc. 2020 Oct 21;13:1203-1213. doi: 10.2147/JMDH.S277133. PMID: 33116565; PMCID: PMC7585795.
- WHO. Mask use in the context of COVID-19. World Heal Organ [Internet]. 2020;(December):1–10. Available from: https://www.who.int/publications/i/item/advice-on-the-use-of-masks-in-the-community-during-home-care-and-in-healthcare-settings-in-the-context-of-the-novel-coronavirus-(2019-ncov)-outbreak
- NPHEOC. NATIONAL PUBLIC HEALTH EMERGENCY OPERATION CENTER ( PHEOC ), ETHIOPIA COVID-19 PANDEMIC PREPAREDNESS AND RESPONSE IN ETHIOPIA Subject of focus : SARS-CoV-2 new Variant of Concern Vaccination against COVID-19 in Ethiopia. 2021;(November):1–18.
- WHO Regional Office for Africa. Weekly Bulletin on Outbreaks. 2020;(August):1–20. Available from: https://apps.who.int/iris/bitstream/handle/10665/331023/OEW07-1016022020.pdf
- Karim SSA. What We Do & Don’t Know About The Omicron Variant [Internet]. SA Corona Virus Online Portal. Available from: https://sacoronavirus.co.za/2021/11/29/presentation-what-we-do-dont-know-about-the-omicron-variant-salim-s-abdool-karim-frs/
- Talic S, Shah S, Wild H, Gasevic D, Maharaj A, Ademi Z, Li X, Xu W, Mesa-Eguiagaray I, Rostron J, Theodoratou E, Zhang X, Motee A, Liew D, Ilic D. Effectiveness of public health measures in reducing the incidence of covid-19, SARS-CoV-2 transmission, and covid-19 mortality: systematic review and meta-analysis. BMJ. 2021 Nov 17;375:e068302. doi: 10.1136/bmj-2021-068302. Erratum in: BMJ. 2021 Dec 3;375:n2997. PMID: 34789505.
- College Of Health Sciences School Of Nursing And Midwifery Postgraduate Program Nurses Knowledge , Attitude And Towards Face Mask And Its Associated Factors Covid-19 Pandemic In Selected Governmental Hospitals , Addis Ababa , Ethiopia , By : Asmeret Leake. 2021;
- Facemask reduces 53% [Internet]. Available from: https://www.newshub.co.nz/home/new-zealand/2021/11/covid-19-global-study-shows-mask-wearing-decreases-virus-prevalence-by-53-percent.html
- Missoni E, Armocida B, Formenti B. Face Masks for All and All for Face Masks in the COVID-19 Pandemic: Community Level Production to Face the Global Shortage and Shorten the Epidemic. Disaster Med Public Health Prep. 2021 Feb;15(1):e29-e33. doi: 10.1017/dmp.2020.207. Epub 2020 Jun 24. Erratum in: Disaster Med Public Health Prep. 2021 Feb;15(1):e50. PMID: 32576310; PMCID: PMC7371839.
- Al Naam YA, Elsafi SH, Alkharraz ZS, Alfahad OA, Al-Jubran KM, Al Zahrani EM. Community practice of using face masks for the prevention of COVID-19 in Saudi Arabia. PLoS One [Internet]. 2021;16(2 February):1–12. Available from: http://dx.doi.org/10.1371/journal.pone.0247313
- Molla KA, Abegaz SB. Community knowledge, attitude and practices to SARS-CoV-2 disease 2019 (COVID-19): A cross-sectional study in Woldia town, Northeast Ethiopia. PLoS One [Internet]. 2021;16(4 April):1–14. Available from: http://dx.doi.org/10.1371/journal.pone.0250465
- Seid Yimer T, Gebrehana Belay H. Knowledge and Practice of Health Care Providers Towards Proper Face Mask Utilization to Minimize the Extent of COVID-19 Infection in Amhara Region Referral Hospitals, Ethiopia. J Multidiscip Healthc. 2021 Jun 28;14:1583-1591. doi: 10.2147/JMDH.S306253. PMID: 34234446; PMCID: PMC8253934.
- Tadesse T, Tesfaye T, Alemu T, Haileselassie W. Healthcare Worker's Knowledge, Attitude, and Practice of Proper Face Mask Utilization, and Associated Factors in Police Health Facilities of Addis Ababa, Ethiopia. J Multidiscip Healthc. 2020 Oct 21;13:1203-1213. doi: 10.2147/JMDH.S277133. PMID: 33116565; PMCID: PMC7585795.
- EMG-NERVTAG, Bundgaard H, Bundgaard JS, Raaschou-Pedersen DET, von Buchwald C, Todsen T, et al. Utilization of personal protective equipment and associated factors among Kombolcha Textile Factory workers, Kombolcha, Ethiopia: A cross-sectional study. AAS Open Res [Internet]. 2020;2020(6):1–12. Available from: https://royalsociety.org/-/media/policy/projects/set-c/set-c-facemasks.pdf
- Getahun TK. Mask Utilization : Knowledge , Attitude and Practice of Addis Ababa Dwellers on Usage of Different Masks in Combating COVID 19 Pandemic. 2021;9(4):100–6.
- Mehmet N, Al-Abed A abed AA, Gökler ME, Elengoe A, Ünal E, Mollahaliloğlu S. Knowledge, attitudes and practices regarding COVID-19 among the Turkish and Malaysian general populations during lockdown: A cross-sectional online survey. Ethiop J Heal Dev. 2020;34(4):243–52.
- Kassa AM, Mekonen AM, Yesuf KA, Woday Tadesse A, Bogale GG. Knowledge level and factors influencing prevention of COVID-19 pandemic among residents of Dessie and Kombolcha City administrations, North-East Ethiopia: a population-based cross-sectional study. BMJ Open. 2020 Nov 14;10(11):e044202. doi: 10.1136/bmjopen-2020-044202. PMID: 33191269; PMCID: PMC7668362.
- Lee M, Kang BA, You M. Knowledge, attitudes, and practices (KAP) toward COVID-19: a cross-sectional study in South Korea. BMC Public Health. 2021 Feb 5;21(1):295. doi: 10.1186/s12889-021-10285-y. PMID: 33546644; PMCID: PMC7863060.
- O'Dowd K, Nair KM, Forouzandeh P, Mathew S, Grant J, Moran R, Bartlett J, Bird J, Pillai SC. Face Masks and Respirators in the Fight against the COVID-19 Pandemic: A Review of Current Materials, Advances and Future Perspectives. Materials (Basel). 2020 Jul 29;13(15):3363. doi: 10.3390/ma13153363. PMID: 32751260; PMCID: PMC7435473.
- Shibesh BF, Minyiwab GW, Admas AB. Community ’ s Mask Wearing Practice and Its Associated Factors for COVID-19 prevention in Metropolitan Town ,. 2021;18(December 2019):378–83.
- Policy H, Asmelash D, Fasil A, Tegegne Y, Akalu TY, Ferede HA, et al. Proof cover sheet. 2020;
- Nuriye Hajiso, S., Lette Wodera, A., Abebe Gebretsadik, L., and Sidamo Summoro T. Patients Satisfaction and its Associated Factors in Rural Health Center, Shashogo District, Southern Ethiopia: A Cross Sectional Study. Prim Heal Care Open Access. 2019;9(2):7.
- Abid K, Bari Y, Ziadi T, Khambati Z, Younus M, Hasan A, et al. Adherence of facemask during Covid pandemic among South Asian countries-An observational study. 2020;1–8. Available from: https://doi.org/10.21203/rs.3.rs-113617/v1
- Haftom M, Petrucka P, Gemechu K, Mamo H, Tsegay T, Amare E, Kahsay H, Gebremariam A. Knowledge, Attitudes, and Practices Towards COVID-19 Pandemic Among Quarantined Adults in Tigrai Region, Ethiopia. Infect Drug Resist. 2020 Oct 20;13:3727-3737. doi: 10.2147/IDR.S275744. PMID: 33116693; PMCID: PMC7585797.
- Kassie BA, Adane A, Kassahun EA, Ayele AS, Belew AK. Poor COVID-19 Preventive Practice among Healthcare Workers in Northwest Ethiopia, 2020. Adv Public Heal. 2020;2020(March).
- Alhazmi A, Ali MHM, Mohieldin A, Aziz F, Osman OB, Ahmed WA. Knowledge, attitudes and practices among people in Saudi Arabia regarding COVID-19: A cross-sectional study. J Public Health Res. 2020 Sep 18;9(3):1867. doi: 10.4081/jphr.2020.1867. PMID: 33042899; PMCID: PMC7520855.
- Yanni Li MPHa, 1, Mingming Liang MPHb, c, 1, Liang Gao MD, PhD d, Mubashir Ayaz Ahmed MDe, John Patrick Uy MDe, Ce Cheng DO f, Qin Zhou PhD g, Chenyu Sun MD Ms e. Since January 2020 Elsevier has created a COVID-19 resource centre with free information in English and Mandarin on the novel coronavirus COVID- 19 . The COVID-19 resource centre is hosted on Elsevier Connect, the company ’ s public news and information. 2020;(January).
- Minyiwab GW. Community ’ s Mask Wearing Practice and Its Associated Factors for COVID-19 prevention in Metropolitan city, Northwest, Ethiopia. 2021;11(7):1–6.
- Haftom M, Petrucka PM. Determinants of Face Mask Utilization to Prevent Covid-19 Pandemic among Quarantined Adults in Tigrai Region, Northern Ethiopia, 2020. Clin Nurs Res. 2021 Sep;30(7):1107-1112. doi: 10.1177/10547738211013219. Epub 2021 May 6. PMID: 33955280; PMCID: PMC8950710.
- Akalu Y, Ayelign B, Molla MD. Knowledge, Attitude and Practice Towards COVID-19 Among Chronic Disease Patients at Addis Zemen Hospital, Northwest Ethiopia. Infect Drug Resist. 2020 Jun 24;13:1949-1960. doi: 10.2147/IDR.S258736. PMID: 32612371; PMCID: PMC7322118.
- Natnael T, Alemnew Y, Berihun G, Abebe M, Andualem A, Ademe S, et al. Facemask wearing to prevent COVID-19 transmission and associated factors among taxi drivers in Dessie City and Kombolcha Town, Ethiopia. PLoS One [Internet]. 2021;16(3 March):1–15. http://dx.doi.org/10.1371/journal.pone.0247954