Abstract
Research Article
Impact of the MELD Scale on Hospital Admissions for Hepatocarcinoma (2000 to 2018), Brazil
Alexandro das Mercês Silva*
Published: 14 March, 2025 | Volume 6 - Issue 1 | Pages: 027-033
Background: The health professional appears to be concerned given the number of questions surrounding the patient’s post-transplant survival, patient selection method, and the continuous search for scores that reflect their reality and reconcile the results they desire with the patient’s expectations. It is from these considerations that the present work was born with the purpose of understanding the reality of patients hospitalized for hepatocellular carcinoma and what adherence to the Model For End-Stage Liver Disease (MELD) criteria meant in Brazil.
Methods: This study is a discrete, univariate time series on emergency hospitalizations that occurred between 2000 and 2018, in the city of São Paulo, Brazil. Python version 3.11 was the software used for statistical treatment and analysis of the time series.
Results: There were 6887 hospitalizations for malignant neoplasm of liver and intrahepatic bile ducts, in the period 2000-2006, of which 2898 were elective and 3915 (56.85%) were urgent in the period. There was an increase of 63.97% in the number of emergency hospitalizations in relation to the period 2000-2006 and 2007-2013. To highlight, in 2013 there were 1270 emergency admissions, which represented an increase of 109.22% in relation to the number of emergency admissions in 2006. The contingency correlation analysis demonstrated a significant association between the variables in which the chi-square value was 82.18, the p-value was 1.24 x 10-19, and the critical value was 3.84 with one degree of freedom. There was a 123.65% increase in the number of hospitalizations for chronic hepatitis, not elsewhere classified, between the periods 2000-2006 and 2007-2013. The chi-square value of the contingency association was 221.22, with a p-value of 4.90 x 10-50, a critical value of 9.488, with a significance level of 5% and one degree of freedom. The study showed an increase in hospitalizations of 21.88% for alcoholic liver disease between the periods 2000-2006 and 2007-2013. In the period 2000-2006, there were 21330 hospitalizations, 19224 of which were urgent (90.13%). In the period 2007-2013, there were 25997 hospitalizations, of which 22,802 (87.71%) occurred urgently. The chi-square value was 68.95, the p-value was 1 x 10-16, and the critical value was 3.84, with one degree of freedom.
Conclusion: The MELD score, as it is sensitive to the patient’s severity, selects those who are at an advanced stage of the disease for liver transplantation. In this scenario, patients do not necessarily have access to outpatient services and begin to attend them regularly when MELD identifies the advanced stage of the disease, opening a gap between prevention, treatment, and rehabilitation.
Read Full Article HTML DOI: 10.29328/journal.jcmhs.1001054 Cite this Article Read Full Article PDF
Keywords:
MELD; Hospitalizations; Hepatocarcinoma
References
- Püschel VAA, Rodrigues AS, Moraes MW. The role of nurses in obtaining organs for transplantation in São Paulo: a legal and bioethical approach. The World of Health Magazine. 2002;26(1).
- Law No. 9434 of February 4, 1997. Provides for the removal of organs, tissues, and parts of the human body for transplantation and treatment purposes and contains other provisions. Official Gazette of the Federative Republic of Brazil. Brasília, February 5, 1997; Section 1:2191.
- Andraus W, Haddad L, Rocha-Santos V, D'Albuquerque LAC. Analysis of organ allocation systems for digestive system transplants in Brazil. Medicine (Ribeirão Preto). 2013;46(3):237-42. Available from: https://doi.org/10.11606/issn.2176-7262.v46i3p237-242
- Ordinance GM No. 2115 of November 20, 2001. Creates, within the scope of the Secretariat of Health Assistance/National Transplant System, a Working Group with the purpose of studying and suggesting to the Ministry of Health the formulation, review, updating, and improvement of the standards related to the criteria for inclusion of patients who are candidates for liver transplantation in the Single Lists of the states, as well as inclusion criteria for the distribution/allocation of livers collected for transplantation purposes. Official Gazette of the Federative Republic of Brazil, Brasília, 2001. Available from: https://bvsms.saude.gov.br/bvs/saudelegis/gm/2001/prt2115_20_11_2001.html
- Ordinance GM No. 541 of March 14, 2002. Approves the criteria for Registration of Liver Recipients – Cadaver Donors, in the Technical Registry of Liver Recipients – “single list” – of the Organ Notification, Procurement and Distribution Centers – CNCDO. Official Gazette of the Federative Republic of Brazil, Brasília. 2005. Available from: https://bvsms.saude.gov.br/bvs/saudelegis/gm/2002/prt0541_14_03_2002.html
- Machado AGS. Impact of implementing the MELD score on liver allocation and liver transplant results: the experience of a Brazilian center. [Dissertation]. [Porto Alegre]: Federal University of Health Sciences of Porto Alegre. 2011;83.
- GM Ordinance No. 1160 of 2006. Modifies the criteria for distribution of livers from deceased donors for transplantation, implementing the criterion of severity of the patient's clinical condition. Official Gazette of the Federative Republic of Brazil, Brasília, 2006. Available from: https://bvsms.saude.gov.br/bvs/saudelegis/gm/2006/prt1160_29_05_2006_comp.html
- Moraes ACO, Oliveira PC, Fonseca-Neto OCL. Impact of the MELD score on liver allocation and liver transplant outcomes: an integrated review. ABCD Brazilian Archive of Digestive Surgery. 2017;30(1):65-68. Available from: https://doi.org/10.1590/0102-6720201700010018
- Kamath PS, Wiesner RH, Malinchoc M, Kremers W, Therneau TM, Kosberg CL, et al. Predict survival in patients with end-stage liver disease. Hepatology. 2001;33(2). Available from: https://doi.org/10.1053/jhep.2001.22172
- Wiesner R, Edwards E, Freeman R, Harper A, Kim R, Kamath P, et al. Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology. 2003;124(1):91-96. Available from: https://doi.org/10.1053/gast.2003.50016
- Lombardi AC, Mente ED, Sankarankutty AK, Souza FF, Teixeira AC, Cagnolati D, et al. Analysis of 83 consecutive liver transplants performed at a tertiary care reference hospital in the interior of the state of São Paulo. Acta Cirúrgica Brasileira. 2011;26(6). Available from: https://doi.org/10.1590/s0102-86502011000600020
- Malinis MF, Chen S, Allore HG, Quagliarello VJ. Outcomes among older adult liver transplantation recipients in the Model of End Stage Liver Disease (MELD) Era. Ann Transplant. 2014;19:478-487. Available from: https://doi.org/10.12659/aot.890934
- Mattos AZ, Mattos AA, Sacco FKF, Hoppe L, Oliveira DMS. Analysis of the survival of cirrhotic patients enlisted for liver transplantation in the pre- and post-MELD era in Southern Brazil. Arq Gastroenterol. 2014;51(1). Available from: https://doi.org/10.1590/s0004-28032014000100010
- Sharpton SR, Feng S, Hameed B, Yao F, Lai JC. Combined effects of recipient age and Model for End-Stage Liver Disease score on liver transplantation outcomes. Transplantation. 2014;98(5):557-562. Available from: https://doi.org/10.1097/tp.0000000000000090
- Freitas AC, Shiguihara RS, Monteiro RT, Pazeto TL, Coelho JCU. Comparative study on liver transplantation with and without hepatocellular carcinoma with cirrhosis: Analysis of MELD, waiting time and survival. ABCD Arq Bras Cir Dig. 2016;29(1):21-25. Available from: https://doi.org/10.1590/0102-6720201600010006
- Bajaj JS, Reddy KR, Tandon P, Wong F, Kamath PS, Garcia-Tsao G, et al. The three-month readmission rate remains unacceptably high in a large North American cohort of cirrhotic patients. Hepatology. 2016 Jul;64(1):200-208. Available from: https://doi.org/10.1002/hep.28414
- Billings J, Blunt I, Steventon A, Georghiou T, Lewis G, Bardsley M. Development of a predictive model to identify inpatients at risk of re-admission within 30 days of discharge (PARR-30). BMJ Open. 2012;2(4):1-9. Available from: https://doi.org/10.1136/bmjopen-2012-001667
- Volk ML, Tocco RS, Bazick J, Rakoski MO, Lok AS. Hospital re-admissions among patients with decompensated cirrhosis. Am J Gastroenterol. 2012;107(2):247-252. Available from: https://doi.org/10.1038/ajg.2011.314
- Rosenstengle C, Kripalani S, Rahimi RS. Hepatic encephalopathy and strategies to prevent readmission from inadequate transitions of care. J Hosp Med. 2022;17:S17-S23. Available from: https://doi.org/10.1002/jhm.12896
- Abou-Alfa GK, Jarnagin W, Lowery M, D'Angelica M, Brown K, Ludwig E, et al. Liver and bile duct cancer. In: Neiderhuber JE, Armitage JO, Doroshow JH, Kastan MB, Tepper JE, editors. Abeloff’s Clinical Oncology. 5th ed. Philadelphia, PA: Elsevier; 2014:1373-1395. Available from: https://synapse.mskcc.org/synapse/works/114787
- Patel T, Borad MJ. Carcinoma of the biliary tree. In: DeVita VT, Lawrence TS, Rosenberg SA, eds. DeVita, Hellman, and Rosenberg’s Cancer: Principles and Practice of Oncology. 10th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2015:715-735. Available from: https://mayoclinic.elsevierpure.com/en/publications/cancer-of-the-biliary-tree
- National Comprehensive Cancer Network. Clinical Practice Guidelines in Oncology (NCCN Guidelines®), Biliary Tract Cancers, Version 2.2024. Accessed on 16 August, 2024. Available from: https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1514
- Silva MJ, Rosa MV, Nogueira PJ, Calina F. Ten years of hospital admissions for liver cirrhosis in Portugal. Eur J Gastroenterol Hepatol. 2015;27(11):1320-1326. Available from: https://doi.org/10.1097/meg.0000000000000449
- Armstrong PR, Ring E, MacNicholas R. A decade of rising alcoholic liver disease hospital admissions and deaths in Irish hospitals, 2007-2016: a retrospective cross-sectional analysis. Eur J Gastroenterol Hepatol. 2022;34(6):671-677. Available from: https://doi.org/10.1097/meg.0000000000002339
- Simmons OL, Feng Y, Parikh ND, Singal AG. Primary care provider practice patterns and barriers to hepatocellular carcinoma surveillance. Clin Gastroenterol Hepatol. 2019;17(4):766-773. Available from: https://doi.org/10.1016/j.cgh.2018.07.029
- Moya LC. Spectrum of alcoholic liver disease: a review of pathophysiology and clinical repercussions. Brazilian J Health Rev. 2022;5(4):13904-13927. Available from: https://doi.org/10.34119/bjhrv5n4-159
- Orman ES, Odena G, Bataller RS. Alcoholic liver disease: pathogenesis, management, and novel targets for therapy. J Gastroenterol Hepatol. 2013;1(1):77-84. Available from: https://doi.org/10.1111/jgh.12030
- Sanyal AJ, Bosch J, Blei A, Arroyo V. Portal hypertension and its complications. Gastroenterology. 2008;134(6):1715-1728. Available from: https://doi.org/10.1053/j.gastro.2008.03.007
- Griswold MG, collaborators. Alcohol use and burden for 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease study 2016. Lancet. 2018;392(22):1015-1035. Available from: https://www.thelancet.com/article/S0140-6736(18)31310-2/fulltext
- Billings J, Parikh N, Mijanovich T. Emergency department use in New York City: a substitute for primary care? The Commonwealth Fund. 2000 Nov;(433):1-5. Available from: https://pubmed.ncbi.nlm.nih.gov/11665698/
- Billings J, Parikh N, Mijanovich. Emergency department use: the New York story. The Commonwealth Fund. 2000;(434):1-12. Available from: https://www.commonwealthfund.org/sites/default/files/documents/___media_files_publications_issue_brief_2000_nov_emergency_room_use__the_new_york_story_billings_nystory_pdf.pdf
- Billings J, Parikh N, Mijanovich. Emergency department use in New York City: a survey of Bronx patients. The Commonwealth Fund. 2000;(435):1-5. Available from: https://pubmed.ncbi.nlm.nih.gov/11665700/
- Billings JB, Raven MC. Dispelling an urban legend: frequent emergency department users have substantial burden of disease. Health Aff. 2013;32(12):2099-2108. Available from: https://doi.org/10.1377/hlthaff.2012.1276
- Raven MC, Carrier ER, Lee J, Billings JC, Marr M, Gourevitch MN. Substance use treatment barriers for patients with frequent hospital admissions. J Subst Abuse Treat. 2010;38(1):22-30. Available from: https://doi.org/10.1016/j.jsat.2009.05.009
- An C, Choi YA, Choi D, Paik YH, Ahn AH, Kim M, et al. Growth rate of early-stage hepatocellular carcinoma in patients with chronic liver disease. Clin Mol Hepatol. 2015;21(3):279-286. Available from: https://doi.org/10.3350/cmh.2015.21.3.279
- Debes JD, Chan AJ, Baderramo D, Kikuchi L, Ballerga EG, Prieto JE, et al. Hepatocellular carcinoma in South America: evaluation of risk factors, demographics and therapy. Liver Int. 2008;38(1):136-143. Available from: https://doi.org/10.1111/liv.13502
- Mukthinuthalapati VV, Akinyeye S, Fricker ZP, Syed M, Orman ES, Nephew L, et al. Early predictors of outcomes of hospitalization for cirrhosis and assessment of the impact of race and ethnicity at safety net hospitals. PLoS One. 2019;14(3):e211811. Available from: https://doi.org/10.1371/journal.pone.0211811
- Mendes BC, Oderich GS, Macedo TA, Moreira RK. Ischemic liver lesions mimicking neoplasm in a patient with severe chronic mesenteric ischemia. J Vasc Surg Cases. 2015;1(2):144-147. Available from: https://doi.org/10.1016/j.jvsc.2015.03.020
- Munter BT, Boyd AR, Tchani R, Gray JN, Ramsey PS. Hepatic infarction in pregnancy: a systematic review. Am J Obstet Gynecol MFM. 2024;6(6):1-9. Available from: https://doi.org/10.1016/j.ajogmf.2024.101377
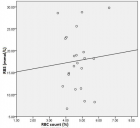
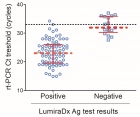
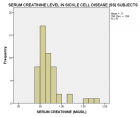
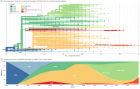
Figures:

Figure 1

Figure 2

Figure 3

Figure 4

Figure 5

Figure 6

Figure 7

Figure 8

Figure 9
Similar Articles
-
Impact of the MELD Scale on Hospital Admissions for Hepatocarcinoma (2000 to 2018), BrazilAlexandro das Mercês Silva*. Impact of the MELD Scale on Hospital Admissions for Hepatocarcinoma (2000 to 2018), Brazil. . 2025 doi: 10.29328/journal.jcmhs.1001054; 6: 027-033
Recently Viewed
-
Evaluation of Long-term Antithrombotic Management for Atrial Fibrillation Patients with a History of Coronary Stent ImplantationKirsten Vyhmeister, Paul Gavaza, Murphy Nguyen, Grace Kang, Huyentran N Tran*. Evaluation of Long-term Antithrombotic Management for Atrial Fibrillation Patients with a History of Coronary Stent Implantation. Ann Clin Hypertens. 2024: doi: 10.29328/journal.ach.1001035; 8: 001-006
-
Call to Action! Hypertension and Dyslipidemia in Mexico: Underestimated Deadly DuoMartin Rosas-Peralta,Héctor Galván-Oseguera,Luis Alcocer,Humberto Álvarez-López,Ernesto Cardona-Muñoz,Silvia Palomo-Piñón,Enrique Díaz-Díaz,Adolfo Chávez-Mendoza,José Manuel Enciso-Muñoz. Call to Action! Hypertension and Dyslipidemia in Mexico: Underestimated Deadly Duo. Ann Clin Hypertens. 2024: doi: 10.29328/journal.ach.1001036; 8: 007-010
-
Sexual Dimorphism in the Length of the Corpus Callosum in CadaverShahnaj Pervin*,Nasaruddin A,Irfan M,Annamalai L. Sexual Dimorphism in the Length of the Corpus Callosum in Cadaver. J Neurosci Neurol Disord. 2024: doi: 10.29328/journal.jnnd.1001104; 8: 126-129
-
Analysis of Psychological and Physiological Responses to Snoezelen Multisensory StimulationLucia Ludvigh Cintulova,Jerzy Rottermund,Zuzana Budayova. Analysis of Psychological and Physiological Responses to Snoezelen Multisensory Stimulation. J Neurosci Neurol Disord. 2024: doi: 10.29328/journal.jnnd.1001103; 8: 115-125
-
Awareness level on the relevance of forensics in criminal investigation in NigeriaOmorogbe Owen Stephen,Orhue Osazee Kelvin,Ehikhamenor Edeaghe,Nwawuba Stanley Udogadi*. Awareness level on the relevance of forensics in criminal investigation in Nigeria. J Forensic Sci Res. 2021: doi: 10.29328/journal.jfsr.1001028; 5: 053-057
Most Viewed
-
Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth EnhancersH Pérez-Aguilar*, M Lacruz-Asaro, F Arán-Ais. Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth Enhancers. J Plant Sci Phytopathol. 2023 doi: 10.29328/journal.jpsp.1001104; 7: 042-047
-
Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case PresentationJulian A Purrinos*, Ramzi Younis. Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case Presentation. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001099; 8: 075-077
-
Feasibility study of magnetic sensing for detecting single-neuron action potentialsDenis Tonini,Kai Wu,Renata Saha,Jian-Ping Wang*. Feasibility study of magnetic sensing for detecting single-neuron action potentials. Ann Biomed Sci Eng. 2022 doi: 10.29328/journal.abse.1001018; 6: 019-029
-
Pediatric Dysgerminoma: Unveiling a Rare Ovarian TumorFaten Limaiem*, Khalil Saffar, Ahmed Halouani. Pediatric Dysgerminoma: Unveiling a Rare Ovarian Tumor. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001087; 8: 010-013
-
Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative reviewKhashayar Maroufi*. Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative review. J Sports Med Ther. 2021 doi: 10.29328/journal.jsmt.1001051; 6: 001-007

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."