Abstract
Research Article
Prevalence and Risk Factors to Preterm Labor through a Study in Jiblah University Hospital, Ibb, Governorate, Yemen
Afaf Alsharif*, Zainab Said, Fatima Mokabes, Leena Ameen, Alya Alqadri, Thekra Musaed, Bushra Musaed, Ala’a Ahmed and Halaa Rigih
Published: 18 February, 2025 | Volume 6 - Issue 1 | Pages: 020-026
Background: Preterm Birth (PTB) is the largest direct cause of neonatal mortality and the second leading cause of under-five mortality following pneumonia. Although there are studies conducted before, the magnitude of PTB remains a major issue in most developing countries including Yemen. Therefore, this study aims to assess the prevalence and associated factors of premature birth among newborns delivered in Jiblah University Hospital in Ibb governorate, Yemen.
Objectives: No studies have previously been conducted about preterm labour in Jiblah University Hospital in Ibb governorate, Yemen.
Methods: This retrospective observational study was conducted in the Department of Obstetrics & Gynecology, Jiblah University Hospital in Ibb Governorate, from 1 December 2023 to 29 February 2024.
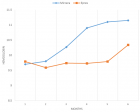
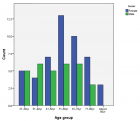
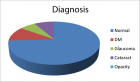
Results: A total of 1350 pregnancies, 252 (18.67%) were preterm deliveries and 1089 (80.66%) were full-term deliveries at Jiblah University Hospital, Ibb. Our study shows the distribution of participants based on socio-demographic factors. The data that out of the total 252 female participants, with ages mean ± std = 27.43 ± 6.34 roughly 18.67% experienced preterm deliveries. Our study demonstrates that several factors are significantly linked to preterm birth, including the number of siblings, blood pressure, gravida, and abortion number, where the Chi-square p - value was < 0.05. On the other hand, the results from the logistic regression analysis indicated the predictive potential of certain socio-demographic factors in relation to preterm birth.
Conclusion: In this study, the number of siblings, blood pressure, gravida, and abortion number are the risk factors for premature delivery. Recognizing the most common risk factors for PTB will help to increase awareness about high-risk pregnancy, improve the preventive measures of preterm risk factors, and modify preterm care protocol in nurseries.
Read Full Article HTML DOI: 10.29328/journal.jcmhs.1001053 Cite this Article Read Full Article PDF
Keywords:
Preterm birth; Risk factors
References
- Blencowe H, Cousens S, Oestergaard MZ, Chou D, Moller AB, Narwal R, et al. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet (London, England). 2012;379(9832):2162–2172. Available from: https://doi.org/10.1016/S0140-6736(12)60820-4
- Hui D, Liu G, Kavuma E, Hewson SA, McKay D, Hannah ME. Preterm labour and birth: a survey of clinical practice regarding use of tocolytics, antenatal corticosteroids, and progesterone. J Obstet Gynaecol Can. 2007;29(2):117–124. Available from: https://doi.org/10.1016/S1701-2163(16)32384-2
- Bafghi AS, Bahrami E, Sekhavat L. Comparative study of vaginal versus intramuscular progesterone in the prevention of preterm delivery: a randomized clinical trial. Electron Physician. 2015;7(6):1301–1309. Available from: https://doi.org/10.14661/1301
- Morrison JJ, Rennie JM. Clinical, scientific, and ethical aspects of fetal and neonatal care at extremely preterm periods of gestation. Br J Obstet Gynaecol. 1997;104(12):1341–1350. Available from: https://doi.org/10.1111/j.1471-0528.1997.tb11002.x
- WHO [World Health Organization]. Preterm birth. Fact sheet N363. [cited 2015 Nov 15]. Available from: https://www.who.int/mediacentre/%20factsheets/fs363/en/
- Gill SV, May-Benson TA, Teasdale A, Munsell EG. Birth and developmental correlates of birth weight in a sample of children with potential sensory processing disorder. BMC Pediatr. 2013;13:29. Available from: https://doi.org/10.1186/1471-2431-13-29
- World Health Organization (WHO). Preterm birth. Retrieved from: https://www.who.int/news-room/fact-sheets/detail/preterm-birth
- Chyi LJ, Lee HC, Hintz SR, Gould JB, Sutcliffe TL. School outcomes of late preterm infants: special needs and challenges for infants born at 32 to 36 weeks gestation. J Pediatr. 2008;153(1):25–31. Available from: https://doi.org/10.1016/j.jpeds.2008.01.027
- Liu L, Johnson HL, Cousens S, Perin J, Scott S, Lawn JE, et al. Child Health Epidemiology Reference Group of WHO and UNICEF. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet (London, England). 2012;379(9832):2151–2161. Available from: https://doi.org/10.1016/S0140-6736(12)60560-1
- Eichenwald EC, Stark AR. Management and outcomes of very low birth weight. N Engl J Med. 2008;358(16):1700–1711. Available from: https://doi.org/10.1056/NEJMra0707601
- Dolatian M, Mirabzadeh A, Forouzan AS, Sajjadi H, Alavimajd H, Mahmoodi Z, Moafi F. Relationship between structural and intermediary determinants of health and preterm delivery. J Reprod Infertil. 2014;15(2):78–86. Available from: https://pubmed.ncbi.nlm.nih.gov/24918080/
- Ibb, Yemen Metro Area Population 1950-2024. 2023. Accessed: 2023-10-05. Available from: https://www.macrotrends.net/cities/23745/ibb/population
- Hassen JA, Handiso MN, Admassu BW. Predictors of preterm birth among mothers who gave birth in Silte zone public hospitals, southern Ethiopia. J Pregnancy. 2021;2021:1706713. Available from: https://doi.org/10.1155/2021/1706713
- Pusdekar YV, Patel AB, Kurhe KG, Bhargav SR, Thorsten V, Garces A, et al. Rates and risk factors for preterm birth and low birth weight in the global network sites in six low- and low-middle-income countries. Reprod Health. 2020;17:187. Available from: https://doi.org/10.1186/s12978-020-01029-z
- Sehati-Shaghaie F, Ghuchazade M, Asdolaie M, Farzolapur F. Prevalence and risk factors of preterm labor in health education centers of Ardabil province (2009–2010). Nurs Midwifery J. 2010;16:22–30.
- Sohrabi D, Ghanbari-Gorkani M. A survey on risk factors and outcomes of women with preterm labor admitted to Valieasr hospital in Zanjan. J Urmia Nurs Midwifery Fac. 2011;9:84–89. Available from: https://unmf.umsu.ac.ir/browse.php?a_id=306&sid=1&slc_lang=en
- Afrakhteh M, Ebrahimi S, Valaei N. Prevalence of preterm delivery and related factors in females referring to Shohada Tajrish hospital, 1995–99. Pejouhandeh. 2002;7:341–344. Available from: https://www.semanticscholar.org/paper/PREVALENCE-OF-PRETERM-DELIVERY-AND-ITS-RELATED-IN-Afrakhteh-Ebrahimi/f3dc0b5b004d47b634ecbf2575025d3cdd8fd4fa
- Jandaghi G, Khalajinia Z, Moghadam PS. Contribution of maternal demographic and medical factors to the risk of prematurity in Qom hospitals. Maced J Med Sci. 2011;4:60–63. Available from: https://www.cabidigitallibrary.org/doi/pdf/10.5555/20113103921
- Martin JA, Hamilton BE, Osterman MJ, Curtin SC, Matthews TJ. Births: final data for 2013. Nat Vital Stat Rep. 2015;64:1–65. Available from: https://pubmed.ncbi.nlm.nih.gov/25603115/
- Khoshnood-Shariati M, Karimi Z, Rezaienejad M, Basiri A, Torkestani F, Gargari SS. Perinatal complications associated with preterm deliveries at 24 to 33 weeks and 6 days gestation (2011–2012): a hospital-based retrospective study. Iran J Reprod Med. 2015;13:697–702. Available from: https://pubmed.ncbi.nlm.nih.gov/26730244/
- Kildea SV, Gao Y, Rolfe M, Boyle J, Tracy S, Barclay LM. Risk factors for preterm, low birthweight and small for gestational age births among Aboriginal women from remote communities in northern Australia. Women Birth. 2017;30(5):398–405. Available from: https://doi.org/10.1016/j.wombi.2017.03.003
- Anderson C, Smitherman AB, Engel SM, Nichols HB. Modifiable and nonmodifiable risk factors for preterm delivery among adolescent and young adult cancer survivors. Cancer Causes Control. 2018;29(2):289–95. Available from: https://doi.org/10.1007/s10552-017-0992-x
- Shah R, Mullany LC, Darmstadt GL, Mannan I, Rahman SM, Talukder RR, et al. Incidence and risk factors of preterm birth in a rural Bangladeshi cohort. BMC Pediatr. 2014;14:112. Available from: https://doi.org/10.1186/1471-2431-14-112
- Gebreslasie K. Preterm birth and associated factors among mothers who gave birth in Gondar town health institutions. Adv Nurs. 2016;2016(1):4703138. Available from: https://doi.org/10.1155/2016/4703138
- Wagura P, Wasunna A, Laving A, Wamalwa D, Ng'ang'a P. Prevalence and factors associated with preterm birth at Kenyatta National Hospital. BMC Pregnancy Childbirth. 2018;18(1):1–8. Available from: https://doi.org/10.1186/s12884-018-1740-2
- Laelago T, Yohannes T, Tsige G. Determinants of preterm birth among mothers who gave birth in East Africa: systematic review and meta-analysis. Ital J Pediatr. 2020;46(1):1–14. Available from: https://doi.org/10.1186/s13052-020-0772-1
- Saccone G, Perriera L, Berghella V. Prior uterine evacuation of pregnancy as independent risk factor for preterm birth: a systematic review and meta-analysis. Am J Obstet Gynecol. 2016 May 1;214(5):572–91. Available from: https://doi.org/10.1016/j.ajog.2015.12.044
- Shah PS. Knowledge Synthesis Group on Determinants of LBW/PT births. Parity and low birth weight and preterm birth: a systematic review and meta-analyses. Acta Obstet Gynecol Scand. 2010;89(7):862–875. Available from: https://doi.org/10.3109/00016349.2010.486827
- Babinszki A, Kerenyi T, Torok O, Grazi V, Lapinski RH, Berkowitz RL. Perinatal outcome in grand and great-grand multiparity: effects of parity on obstetric risk factors. Am J Obstet Gynecol. 1999;181(3):669–674. Available from: https://doi.org/10.1016/s0002-9378(99)70511-9
- Guo LJ, Ye RW, Wang GX, Wang J, Li ZW, Ren AG. Birth weight distribution among premature infants and related social factors [Chinese]. Zhonghua Liu Xing Bing Xue Za Zhi. 2009;30(12):1243–1247. Available from: https://pubmed.ncbi.nlm.nih.gov/20193306/
- Reime B, Schuecking BA, Wenzlaff P. Perinatal outcomes of teenage pregnancies according to gravidity and obstetric history. Ann Epidemiol. 2004;14(8):619. Available from: https://doi.org/10.1186/1471-2393-8-4
- Lazdam M, De la Horra A, Pitcher A, Mannie Z, Diesch J, Trevitt C, et al. Elevated blood pressure in offspring born premature to hypertensive pregnancy: is endothelial dysfunction the underlying vascular mechanism? Hypertension. 2010;56(1):159–165. Available from: https://doi.org/10.1161/hypertensionaha.110.150235
- Shingairai AF, Siobán DH, Godfrey BW. Risk factors for prematurity at Harare Maternity Hospital, Zimbabwe. Int J Epidemiol. 2004;33(6):1194–1201. Available from: https://doi.org/10.1093/ije/dyh120
- Covarrubias LO, Aguirre GE, Chapuz JR, May AI, Velázquez JD, Eguiluz ME. Maternal factors associated to prematurity [Spanish]. Ginecol Obstet Mex. 2008;76(9):526–536. Available from: https://pubmed.ncbi.nlm.nih.gov/18798459/
- Sureshbabu RP, Aramthottil P, Anil N, Sumathy S, Varughese SA, Sreedevi A, et al. Risk factors associated with preterm delivery in singleton pregnancy in a tertiary care hospital in South India: a case control study. Int J Womens Health. 2021;13:369–377. Available from: https://doi.org/10.2147/ijwh.s282251
- Chauhan N, Purohit RC, Rawat U. Analysis of etiology and outcome of preterm labour in tertiary health centre of Uttarakhand. Sch J App Med Sci. 2016;4:740–743.
- Prakash SA, Rasquinha S, Rajaratnam A, Lavanya S. Analysis of risk factors and outcome of preterm labor. Int J Eng Sci. 2016;6(8):2602–2604.
Figures:
Similar Articles
-
Prevalence of Risk factors of Non Communicable Diseases amongst Medical Students, Kanpur, Uttar Pradesh, IndiaLakshmi Singh*, Anju Gahlot, Atul Kumar Singh. Prevalence of Risk factors of Non Communicable Diseases amongst Medical Students, Kanpur, Uttar Pradesh, India. . 2024 doi: 10.29328/journal.jcmhs.1001048; 5: 057-061
-
Prevalence and Risk Factors to Preterm Labor through a Study in Jiblah University Hospital, Ibb, Governorate, YemenAfaf Alsharif*,Zainab Said,Fatima Mokabes,Leena Ameen,Alya Alqadri,Thekra Musaed,Bushra Musaed,Ala’a Ahmed,Halaa Rigih. Prevalence and Risk Factors to Preterm Labor through a Study in Jiblah University Hospital, Ibb, Governorate, Yemen. . 2025 doi: 10.29328/journal.jcmhs.1001053; 6: 020-026
Recently Viewed
-
Clinical and Histopathological Mismatch: A Case Report of Acral FibromyxomaMonica Mishra*,Kailas Mulsange,Gunvanti Rathod,Deepthi Konda. Clinical and Histopathological Mismatch: A Case Report of Acral Fibromyxoma. Arch Pathol Clin Res. 2025: doi: 10.29328/journal.apcr.1001045; 9: 005-007
-
Unconventional powder method is a useful technique to determine the latent fingerprint impressionsHarshita Niranjan,Shweta Rai,Kapil Raikwar,Chanchal Kamle,Rakesh Mia*. Unconventional powder method is a useful technique to determine the latent fingerprint impressions. J Forensic Sci Res. 2022: doi: 10.29328/journal.jfsr.1001035; 6: 045-048
-
Doppler Evaluation of Renal Vessels in Pediatric Patients with Relapse and Remission in Different Categories of Nephrotic SyndromeAmit Nandan Dhar Dwivedi*, Srishti Sharma, OP Mishra, Girish Singh. Doppler Evaluation of Renal Vessels in Pediatric Patients with Relapse and Remission in Different Categories of Nephrotic Syndrome. J Clini Nephrol. 2023: doi: 10.29328/journal.jcn.1001112; 7: 067-072
-
Atlantoaxial subluxation in the pediatric patient: Case series and literature reviewCatherine A Mazzola*,Catherine Christie,Isabel A Snee,Hamail Iqbal. Atlantoaxial subluxation in the pediatric patient: Case series and literature review. J Neurosci Neurol Disord. 2020: doi: 10.29328/journal.jnnd.1001037; 4: 069-074
-
Intelligent Design of Ecological Furniture in Risk Areas based on Artificial SimulationTorres del Salto Rommy Adelfa*, Bryan Alfonso Colorado Pástor*. Intelligent Design of Ecological Furniture in Risk Areas based on Artificial Simulation. Arch Surg Clin Res. 2024: doi: 10.29328/journal.ascr.1001083; 8: 062-068
Most Viewed
-
Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth EnhancersH Pérez-Aguilar*, M Lacruz-Asaro, F Arán-Ais. Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth Enhancers. J Plant Sci Phytopathol. 2023 doi: 10.29328/journal.jpsp.1001104; 7: 042-047
-
Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case PresentationJulian A Purrinos*, Ramzi Younis. Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case Presentation. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001099; 8: 075-077
-
Feasibility study of magnetic sensing for detecting single-neuron action potentialsDenis Tonini,Kai Wu,Renata Saha,Jian-Ping Wang*. Feasibility study of magnetic sensing for detecting single-neuron action potentials. Ann Biomed Sci Eng. 2022 doi: 10.29328/journal.abse.1001018; 6: 019-029
-
Pediatric Dysgerminoma: Unveiling a Rare Ovarian TumorFaten Limaiem*, Khalil Saffar, Ahmed Halouani. Pediatric Dysgerminoma: Unveiling a Rare Ovarian Tumor. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001087; 8: 010-013
-
Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative reviewKhashayar Maroufi*. Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative review. J Sports Med Ther. 2021 doi: 10.29328/journal.jsmt.1001051; 6: 001-007

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."