Abstract
Research Article
Neurovascular Shifts, Sensory Sensitivity, and PMDD in Autistic Women: Exploring Blood Flow Redirection, Mood Dysregulation, and Pain Tolerance during Menstruation
Piper Hutson and James Hutson*
Published: 30 September, 2024 | Volume 5 - Issue 2 | Pages: 062-068
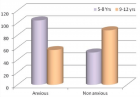
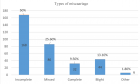
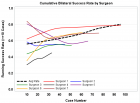
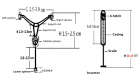
This article examines the relationship between Premenstrual Dysphoric Disorder (PMDD), neurovascular dynamics, and sensory sensitivities in autistic women during menstruation. The redirection of blood flow to the uterus during the menstrual cycle has been found to exacerbate cerebral perfusion deficits in neurodivergent individuals, particularly in the Prefrontal Cortex (PFC), which contributes to the mood dysregulation and emotional instability characteristic of PMDD. Autistic women, who often exhibit heightened sensory sensitivities, experience intensified discomfort during menstruation, as sensory overload and altered pain perception compound the emotional challenges of PMDD. These findings emphasize the need for neurodivergent-friendly menstrual products that mitigate both physical and emotional discomfort. Additionally, innovations using biodegradable materials, smart fabrics, and custom-fit menstrual solutions are discussed as potential breakthroughs to improve the quality of life for autistic women managing PMDD. This research highlights the importance of addressing both neurobiological and sensory aspects when designing interventions for PMDD in neurodivergent populations.
Read Full Article HTML DOI: 10.29328/journal.jcmhs.1001049 Cite this Article Read Full Article PDF
Keywords:
PMDD; Neurovascular dynamics; Autistic women; Sensory sensitivity; Mood dysregulation; Menstrual product innovation
References
- Huang J, Li Q, Lu J, Zhao G. PET/MR: functional and molecular imaging of neurological diseases. Neurosciences. 2023;369.
- Gothe NP, Erlenbach E, Garcia V, Malani R, Voss S, Camacho PB, et al. Yoga, aerobic and stretching exercise effects on neurocognition: randomized controlled trial protocol. Contemp Clin Trials. 2023;131:107240. Available from: https://doi.org/10.1016/j.cct.2023.107240
- Swihart A, Mathew R, Largen J. Menstruation and cerebral blood flow. Biol Psychiatry. 1989;25:654-657. Available from: https://doi.org/10.1016/0006-3223(89)90231-x.
- Favre M, Serrador JM. Sex differences in cerebral autoregulation are unaffected by menstrual cycle phase in young, healthy women. Am J Physiol Heart Circ Physiol. 2019;316(4). Available from: https://doi.org/10.1152/ajpheart.00474.2018
- Li Y, Ma S, Zhang X, Gao L. ASD and ADHD: divergent activating patterns of prefrontal cortex in executive function tasks? J Psychiatr Res. 2024. Available from: https://doi.org/10.1016/j.jpsychires.2024.02.012
- Flynn R. Impact of head injury on cognitive functioning and social cognition in UK-based female rugby players [dissertation]. University of East London; 2024. Available from: https://repository.uel.ac.uk/item/8x2yx
- Ossewaarde L, Hermans EJ, Wingen G, Kooijman S, Johansson I, Bäckström T, et al. Neural mechanisms underlying changes in stress-sensitivity across the menstrual cycle. Psychoneuroendocrinology. 2010;35:47-55. Available from: https://doi.org/10.1016/j.psyneuen.2009.08.011
- Peltonen G, Harrell J, Aleckson B, LaPlante K, Crain M, Schrage W. Cerebral blood flow regulation in women across menstrual phase: differential contribution of cyclooxygenase to basal, hypoxic, and hypercapnic vascular tone. Am J Physiol Regul Integr Comp Physiol. 2016;311(2). Available from: https://doi.org/10.1152/ajpregu.00106.2016
- Arslan R, Yanık D, Pekşen Akça R. Investigation of menstrual hygiene and self-care skills of adolescent girls with autism spectrum disorder: mother views. J Autism Dev Disord. 2024;1-9. Available from: https://link.springer.com/article/10.1007/s10803-024-06446-8
- Manikandan S, Nillni Y, Zvolensky M, Rohan K, Carkeek K, Leyro T. The role of emotion regulation in the experience of menstrual symptoms and perceived control over anxiety-related events across the menstrual cycle. Arch Women Ment Health. 2016;19:1109-1117. Available from: https://doi.org/10.1007/s00737-016-0661-1
- Qian H, Shao M, Wei Z, Zhang Y, Liu S, Chen L, Meng J. Intact painful sensation but enhanced non-painful sensation in individuals with autistic traits. Front Psychiatry. 2024;15:1432149. Available from: https://doi.org/10.3389/fpsyt.2024.1432149
- Zoltowski AR, Failla MD, Quinde-Zlibut JM, Dunham-Carr K, Moana-Filho EJ, Essick GK, et al. Differences in temporal profile of brain responses by pleasantness of somatosensory stimulation in autistic individuals. Somatosens Mot Res. 2023;1-16. Available from: https://doi.org/10.1080/08990220.2023.2294715
- Yasuda Y, Hashimoto R, Nakae A, Kang H, Ohi K, Yamamori H, et al. Sensory cognitive abnormalities of pain in autism spectrum disorder: a case-control study. Ann Gen Psychiatry. 2016;15:1-8. Available from: https://doi.org/10.1186/s12991-016-0095-1
- Liu N, Li Y, Hong Y, Huo J, Chang T, Wang H, et al. Altered brain activities in mesocorticolimbic pathway in primary dysmenorrhea patients of long-term menstrual pain. Front Neurosci. 2023;17:1098573. Available from: https://doi.org/10.3389/fnins.2023.1098573
- Vaughan S, McGlone F, Poole H, Moore D. A quantitative sensory testing approach to pain in autism spectrum disorders. J Autism Dev Disord. 2019;50:1607-1620. Available from: https://doi.org/10.1007/s10803-019-03918-0
- Steward R, Crane L, Roy E, Remington A, Pellicano E. “Life is much more difficult to manage during periods”: autistic experiences of menstruation. J Autism Dev Disord. 2018;48:4287-4292. Available from: https://link.springer.com/article/10.1007/s10803-018-3664-0
- Lundy KM, Fischer AJ, Illapperuma-Wood CR, Schultz B. Understanding autistic youths’ menstrual product preferences and caregivers’ product choices. Autism. 2024;13623613241275280. Available from: https://doi.org/10.1177/13623613241275280
- Moseley R, Druce T, Turner-Cobb J. ‘When my autism broke’: a qualitative study spotlighting autistic voices on menopause. Autism. 2020;24:1423-1437. Available from: https://doi.org/10.1177%2F1362361319901184
- Gray LJ, Durand H. Experiences of dysmenorrhea and its treatment among allistic and autistic menstruators: a thematic analysis. BMC Womens Health. 2023;23(1):288. Available from: https://doi.org/10.1186/s12905-023-02370-8
- Zhang L, Zhao Y, Liu X, Chen J, Sun M, Zhang J, et al. Changes in sex hormones and their interactions are related to pain perception between different menstrual subphases. Am J Physiol Regul Integr Comp Physiol. 2023;325(3). Available from: https://doi.org/10.1152%2Fajpregu.00275.2022
- Pfleeger M, Straneva PA, Fillingim RB, Maixner W, Girdler SS. Menstrual cycle, blood pressure and ischemic pain sensitivity in women: a preliminary investigation. Int J Psychophysiol. 1997;27(2):161-166. Available from: https://doi.org/10.1016/s0167-8760(97)00058-5
- Cervin M, Storch EA, Kendall PC, Herrington JD, Small BJ, Wood JJ, et al. Effects of cognitive-behavioral therapy on core aspects of anxiety in anxious youth with autism. Res Autism Spectr Disord. 2023;107:102221. Available from: https://doi.org/10.1016/j.rasd.2023.102221
- Hellström B, Anderberg UM. Pain perception across the menstrual cycle phases in women with chronic pain. Percept Mot Skills. 2003;96(1):201-211. Available from: https://doi.org/10.2466/pms.2003.96.1.201
- Pergantis P, Drigas A. Sensory integration therapy as an enabler for developing emotional intelligence in children with autism spectrum disorder and the ICT’s role. Braz J Sci. 2023;2(12):53-65. Available from: http://dx.doi.org/10.14295/bjs.v2i12.422
- Steward T, Das P, Malhi GS, Bryant RA, Felmingham KL. Dysfunctional coupling of the parahippocampal cortex and inferior frontal gyrus during memory suppression in posttraumatic stress disorder. Eur Neuropsychopharmacol. 2020;41:146-151. Available from: https://doi.org/10.1016/j.euroneuro.2020.09.634
- Scott K, Schulz S, Moehrle D, Allman B, Cardy J, Stevenson R, et al. Closing the species gap: translational approaches to studying sensory processing differences relevant for autism spectrum disorder. Autism Res. 2021;14:1322-1331. Available from: https://doi.org/10.1002/aur.2533
- Morgan JE. Serum concentrations of protein S100B and the menstrual cycle [dissertation]. Appalachian State University; 2020. Available from: https://libres.uncg.edu/ir/asu/f/Morgan_Jessica_August%202020_Thesis.pdf
- Resham G, Reshmi CR, Nair S, Menon D. Superabsorbent sodium carboxymethyl cellulose membranes based on a new cross-linker combination for female sanitary napkin applications. Carbohydr Polym. 2020;248:116763. Available from: https://doi.org/10.1016/j.carbpol.2020.116763
- Shibly M, Hossain M, Hossain M, Nur M, Hossain M. Development of biopolymer-based menstrual pad and quality analysis against commercial merchandise. Bull Natl Res Cent. 2021;45:1-13. Available from: https://bnrc.springeropen.com/articles/10.1186/s42269-021-00504-2
- Foster J, Montgomery P. A study of environmentally friendly menstrual absorbents in the context of social change for adolescent girls in low- and middle-income countries. Int J Environ Res Public Health. 2021;18. Available from: https://doi.org/10.3390/ijerph18189766
- Woytuk N, Søndergaard M. Biomenstrual: more-than-human design of menstrual care practices. Temes de Disseny. 2022. Available from: http://orcid.org/0000-0002-9884-0205
- Bataglioli RA, Kaur H, Muller J, Geddes E, Champine C, Hsu BB. A naturally derived biomaterial formulation for improved menstrual care. Matter. 2024;7(9):2941-2958. Available from: https://www.cell.com/matter/abstract/S2590-2385(24)00347-3
- Patterson R. The mass customization of sandal outsoles for female size outliers utilizing parametric modeling and 3D printing [dissertation]. Georgia Institute of Technology; 2020. Available from: http://hdl.handle.net/1853/63681
- Greiwe J, Nyenhuis SM. Wearable technology and how this can be implemented into clinical practice. Curr Allergy Asthma Rep. 2020;20:1-10. Available from: https://doi.org/10.1007%2Fs11882-020-00927-3
- Prahl A. Designing wearable sensors for preventative health: an exploration of material, form, and function [dissertation]. University of the Arts London; 2015. Available from: https://ualresearchonline.arts.ac.uk/id/eprint/9077/
- Vogel W. Upcycling invasive species to address social issues: developing a compostable menstrual pad from water hyacinth. Available from: https://digital.library.txst.edu/items/da0e5de2-33e0-470c-960c-fabf2a20c4ab
- Barman J, Tirkey A, Batra S, Paul AA, Panda K, Deka R, et al. The role of nanotechnology-based wearable electronic textiles in biomedical and healthcare applications. Mater Today Commun. 2022;32:104055. Available from: https://doi.org/10.1016/j.mtcomm.2022.104055
- Marzuki I, Sinardi S, Pratama I, Chaerul M, Paserangi I, Mudyawati M, et al. Performance of sea sponges micro symbionts as a biomaterial in biodegradation of naphthalene waste. In: IOP Conference Series: Earth and Environmental Science. 2021;737(1):012016. IOP Publishing. Available from: https://iopscience.iop.org/article/10.1088/1755-1315/737/1/012016
- Martínez-Barbosa ME, Moreno-Corral RA. Washable, reusable, and disposable medical textiles. In: Medical Textiles from Natural Resources. Woodhead Publishing; 2022;717-765. Available from: https://doi.org/10.1016/B978-0-323-90479-7.00017-8
- Reddy K, Taksande A, Kurian B. Harnessing the power of mobile phone technology: screening and identifying autism spectrum disorder with smartphone apps. Cureus. 2024;16(2). Available from: https://doi.org/10.7759%2Fcureus.55004
- Moisanen K, Huhtala S. Smart solutions for wellbeing service development and management-Winternational 6.0. 2024.
- Mancebo CPC. 3D printing and its possible role in the sustainability of the fashion market [dissertation]. 2023.
- Bashari A, Rouhani Shirvan A, Shakeri M. Cellulose-based hydrogels for personal care products. Polymers for Adv Technol. 2018;29(12):2853-2867. Available from: https://doi.org/10.1002/pat.4290
- Tizabi Y, Getachew B, Hauser SR, Tsytsarev V, Manhães AC, da Silva VDA. Role of glial cells in neuronal function, mood disorders, and drug addiction. Brain Sci. 2024;14(6):558. Available from: https://doi.org/10.3390/brainsci14060558
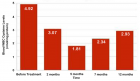
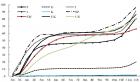
Figures:
Similar Articles
-
Neurovascular Shifts, Sensory Sensitivity, and PMDD in Autistic Women: Exploring Blood Flow Redirection, Mood Dysregulation, and Pain Tolerance during MenstruationPiper Hutson, James Hutson*. Neurovascular Shifts, Sensory Sensitivity, and PMDD in Autistic Women: Exploring Blood Flow Redirection, Mood Dysregulation, and Pain Tolerance during Menstruation. . 2024 doi: 10.29328/journal.jcmhs.1001049; 5: 062-068
Recently Viewed
-
The efficacy of complex Decongestive Physiotherapy in patients with Bilateral Primary Lower Extremity Lymphedema and Untreatable multiple health conditions: A Case ReportHümeyra Kiloatar PT*. The efficacy of complex Decongestive Physiotherapy in patients with Bilateral Primary Lower Extremity Lymphedema and Untreatable multiple health conditions: A Case Report. J Nov Physiother Rehabil. 2017: doi: 10.29328/journal.jnpr.1001011; 1: 093-098
-
Cystoid Macular Oedema Secondary to Bimatoprost in a Patient with Primary Open Angle GlaucomaKonstantinos Kyratzoglou*,Katie Morton. Cystoid Macular Oedema Secondary to Bimatoprost in a Patient with Primary Open Angle Glaucoma. Int J Clin Exp Ophthalmol. 2025: doi: 10.29328/journal.ijceo.1001059; 9: 001-003
-
Metastatic Brain Melanoma: A Rare Case with Review of LiteratureNeha Singh,Gaurav Raj,Akshay Kumar,Deepak Kumar Singh,Shivansh Dixit,Kaustubh Gupta*. Metastatic Brain Melanoma: A Rare Case with Review of Literature. J Radiol Oncol. 2025: doi: ; 9: 050-053
-
Depression as a civilization-deformed adaptation and defence mechanismBohdan Wasilewski*,Olha Yourtsenyuk,Eugene Egan. Depression as a civilization-deformed adaptation and defence mechanism. Insights Depress Anxiety. 2020: doi: 10.29328/journal.ida.1001013; 4: 008-011
-
Drinking-water Quality Assessment in Selective Schools from the Mount LebanonWalaa Diab, Mona Farhat, Marwa Rammal, Chaden Moussa Haidar*, Ali Yaacoub, Alaa Hamzeh. Drinking-water Quality Assessment in Selective Schools from the Mount Lebanon. Ann Civil Environ Eng. 2024: doi: 10.29328/journal.acee.1001061; 8: 018-024
Most Viewed
-
Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth EnhancersH Pérez-Aguilar*, M Lacruz-Asaro, F Arán-Ais. Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth Enhancers. J Plant Sci Phytopathol. 2023 doi: 10.29328/journal.jpsp.1001104; 7: 042-047
-
Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case PresentationJulian A Purrinos*, Ramzi Younis. Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case Presentation. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001099; 8: 075-077
-
Feasibility study of magnetic sensing for detecting single-neuron action potentialsDenis Tonini,Kai Wu,Renata Saha,Jian-Ping Wang*. Feasibility study of magnetic sensing for detecting single-neuron action potentials. Ann Biomed Sci Eng. 2022 doi: 10.29328/journal.abse.1001018; 6: 019-029
-
Pediatric Dysgerminoma: Unveiling a Rare Ovarian TumorFaten Limaiem*, Khalil Saffar, Ahmed Halouani. Pediatric Dysgerminoma: Unveiling a Rare Ovarian Tumor. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001087; 8: 010-013
-
Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative reviewKhashayar Maroufi*. Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative review. J Sports Med Ther. 2021 doi: 10.29328/journal.jsmt.1001051; 6: 001-007

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."