Abstract
Short Review
Senile Cataract
Ragni Kumari*
Published: 02 February, 2024 | Volume 5 - Issue 1 | Pages: 001-007
Cataracts may be described as the opacity of crystalline lenses present in the eye. The translucent crystalline lens is a part of the human eye. It possesses all the physical characteristics of a biconvex lens. The eye’s lens performs similar functions to a camera’s lens. The lens directs light rays entering the eye to the retina’s sensitive layers. Any factor that increases the absorption of scattering of light by the lens reduces its transparency. The opacity of the lens or its capsule, whether developmental or acquired, is called a cataract. Cataracts vary in degree of density and site and assume various forms. Cataract is the leading cause of reversible visual impairment and blindness globally. There are several classifications of cataracts based on morphologic and/or etiologic criteria. However, in epidemiologic studies, the simplified system of three types based on localization of lens opacities is most commonly used: Nuclear cataract is the most common type, followed by cortical cataract and posterior subcapsular cataract. This most prevalent form of acquired cataract, also known as an “age-related cataract,” affects people of both sexes equally and typically develops after age 50. More than 90% of people experience senile cataracts by age 70. Although one eye is almost always afflicted before the other, the disorder is typically bilateral. In the available literature, there is no mention of any such drug that could reverse the opacity of the lens (cataract) once it occurred and make it clear and transparent again.
Only replacement of opaque lenses with artificial transparent Intraocular lens (IOL) is successful treatment of cataracts. This review focuses on senile cataracts and the best possible management of senile cataracts.
Read Full Article HTML DOI: 10.29328/journal.jcmhs.1001041 Cite this Article Read Full Article PDF
Keywords:
Lens; Cataract; Opacity; Age; Crystalline; Senile
References
- National Programme for Control of Blindness &Visual Impairment, Directorate General of Health Services, MHFW, New Delhi. 2019.
- Hall AB, Thompson JR, Deane JS, Rosenthal AR. LOCS III versus the Oxford Clinical Cataract Classification and Grading System for the assessment of nuclear, cortical and posterior subcapsular cataract. Ophthalmic Epidemiol. 1997 Dec;4(4):179-94. doi: 10.3109/09286589709059192. PMID: 9500153.
- Thylefors B. A global initiative for the elimination of avoidable blindness. Indian J Ophthalmol. 1998 Sep;46(3):129-30. PMID: 10085623.
- Thylefors B, Chylack LT Jr, Konyama K, Sasaki K, Sperduto R, Taylor HR, West S; WHO Cataract Grading Group. A simplified cataract grading system. Ophthalmic Epidemiol. 2002 Apr;9(2):83-95. doi: 10.1076/opep.9.2.83.1523. PMID: 11821974.
- Michael R, Bron AJ. The ageing lens and cataract: a model of normal and pathological ageing. Philos Trans R Soc Lond B Biol Sci. 2017; 366: 1278–1292.
- Osnes-Ringen O, Azqueta AO, Moe MC, Zetterström C, Røger M, Nicolaissen B, Collins AR. DNA amage in lens epithelium of cataract patients in vivo and ex vivo. Acta Ophthalmologica. 2013; 91(7): 652–656. doi:10.1111/j.1755-3768.2012.02500.x
- Roberts JE. Ultraviolet radiation as a risk factor for cataract and macular degeneration. Eye Contact Lens. 2011 Jul;37(4):246-9. doi: 10.1097/ICL.0b013e31821cbcc9. PMID: 21617534.
- Balasubramanian D. Ultraviolet radiation and cataract. J Ocul Pharmacol Ther. 2000 Jun;16(3):285-97. doi: 10.1089/jop.2000.16.285. PMID: 10872925.
- Ortwerth BJ, Prabhakaram M, Nagaraj RH, Linetsky M. The relative UV sensitizer activity of purified advanced glycation endproducts. Photochem Photobiol. 1997 Apr;65(4):666-72. doi: 10.1111/j.1751-1097.1997.tb01909.x. PMID: 9114742.
- Roberts J. Screening dyes, drugs, and dietary supplements for ocular phototoxicity. In Photostability of Drugs and Drug Formulations, Second Edition. 2004; 235–254. doi:10.1201/9781420023596.ch11
- Taylor HR, West S, Muñoz B, Rosenthal FS, Bressler SB, Bressler NM. The long-term effects of visible light on the eye. Arch Ophthalmol. 1992 Jan;110(1):99-104. doi: 10.1001/archopht.1992.01080130101035. PMID: 1731731.
- Sliney DH. Intraocular and crystalline lens protection from ultraviolet damage. Eye Contact Lens. 2011 Jul;37(4):250-8. doi: 10.1097/ICL.0b013e31822126d4. PMID: 21670691.
- Shiels A, Bennett TM, Knopf HL, Maraini G, Li A, Jiao X, Hejtmancik JF. The EPHA2 gene is associated with cataracts linked to chromosome 1p. Mol Vis. 2008;14:2042-55. Epub 2008 Nov 12. PMID: 19005574; PMCID: PMC2582197.
- Age-Related Eye Disease Studies (AREDS/AREDS2) | National Eye Institute. 2023. https://www.nei.nih.gov/research/clinical-trials/age-related-eye-disease-studies-aredsareds2
- Khurana A. Comprehensive Ophthalmology. Jaypee Brothers Medical Publishers (P) Ltd. eBooks. 2015. https://doi.org/10.5005/jp/books/12532
Figures:
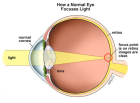
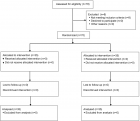
Figure 1
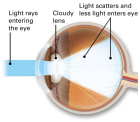
Figure 2
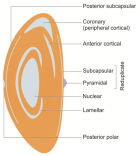
Figure 3
Similar Articles
-
Assessment of knowledge, practice and associated factors towards prevention of novel corona virus among clients attending at Debre Tabor General Hospital, Debre Tabor Town, North West Ethiopia, 2020: Institutional based cross-sectional studyTigabu Desie Emiru*,Tekalign Amera Birlie,Sheganew Fetene Tasew,Abraham Tsedalu Amare,Nigusie Selomon Tibebu,Chalie Marew Tiruneh. Assessment of knowledge, practice and associated factors towards prevention of novel corona virus among clients attending at Debre Tabor General Hospital, Debre Tabor Town, North West Ethiopia, 2020: Institutional based cross-sectional study. . 2020 doi: 10.29328/journal.jcmhs.1001004; 1: 026-034
-
Suicide in teenagers during the COVID-19 pandemic in Cuba: actions for its preventionMaydell Pérez Inerárity*,Claudia Elvira Casamayor Leiza,Julio César Pérez Yero,Brayan Chávez Miguel. Suicide in teenagers during the COVID-19 pandemic in Cuba: actions for its prevention. . 2021 doi: 10.29328/journal.jcmhs.1001007; 2: 001-006
-
Factors influencing referral delay of cancer patients to an oncology unit in the Southern Region of Saudi ArabiaAli M Al Zahrani*,Hatim M Ali,Shaza A Ahmed,Ahmed M Abdelakher,Asma A Al Zahrani,Hatoon Bakhribah. Factors influencing referral delay of cancer patients to an oncology unit in the Southern Region of Saudi Arabia. . 2021 doi: 10.29328/journal.jcmhs.1001012; 2: 025-030
-
Knowledge, attitude and practice towards facemask use amid the COVID-19 pandemic among public transport drivers in Debre-Tabor town, EthiopiaGashaw Mehiret Wubet*,Libsuye Yalgaw Zimamu. Knowledge, attitude and practice towards facemask use amid the COVID-19 pandemic among public transport drivers in Debre-Tabor town, Ethiopia. . 2022 doi: 10.29328/journal.jcmhs.1001013; 3: 001-010
-
Associations of Exercise Habits and Circulatory Dynamics with Peripheral Lower Limb Body Composition in Healthy Community-dwelling Older IndividualsHaruki Kogo*,Yuh Yamashita,Jun Murata. Associations of Exercise Habits and Circulatory Dynamics with Peripheral Lower Limb Body Composition in Healthy Community-dwelling Older Individuals. . 2022 doi: 10.29328/journal.jcmhs.1001017; 3: 027-034
-
Face mask utilization and associated factors in combating COVID-19 pandemic among government employee in Akaki district administration offices, Oromia, Ethiopia, 2022Amenti Teka Geferso*,Derese Desalegn Buta,Adam Sheikh Said,Geleta Merga Duguma. Face mask utilization and associated factors in combating COVID-19 pandemic among government employee in Akaki district administration offices, Oromia, Ethiopia, 2022. . 2022 doi: 10.29328/journal.jcmhs.1001018; 3: 035-047
-
The factors associated with mental health and the impact of COVID-19Linda Martinez*,Rebecca Perley,Salim Alani,Henry O’Lawrence. The factors associated with mental health and the impact of COVID-19. . 2022 doi: 10.29328/journal.jcmhs.1001019; 3: 048-053
-
The effects of exercise intensity on the gut microbiota of college basketball playersHong-xian Deng,Huan-huan Li,Jiu-quan Qiao*,Yan Tong*,Cui-juan Wang,Jiang Liu. The effects of exercise intensity on the gut microbiota of college basketball players. . 2023 doi: 10.29328/journal.jcmhs.1001028; 4: 010-018
-
Clinical profile, prognosis and post COVID-19 Illnesses among attendants to private general practitioner (GP) clinic at Urban Amman Area: a clinical case-series studyEsraa Abuzayed*,Ishtaiwi Abuzayed. Clinical profile, prognosis and post COVID-19 Illnesses among attendants to private general practitioner (GP) clinic at Urban Amman Area: a clinical case-series study. . 2023 doi: 10.29328/journal.jcmhs.1001029; 4: 019-022
-
Hazardous Effects of Malaria for Patients Residing in Low-probability Malaria Areas: A Case Report and Critiques of the Literature for Cerebral MalariaJanvier Nzayikorera*. Hazardous Effects of Malaria for Patients Residing in Low-probability Malaria Areas: A Case Report and Critiques of the Literature for Cerebral Malaria. . 2023 doi: 10.29328/journal.jcmhs.1001038; 4: 076-079
Recently Viewed
-
The Effect of Humidity on Blood Serum Pattern Formation and Blood TransferKelly P Kearse*. The Effect of Humidity on Blood Serum Pattern Formation and Blood Transfer. J Forensic Sci Res. 2023: doi: 10.29328/journal.jfsr.1001048; 7: 040-048.
-
Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case PresentationJulian A Purrinos*, Ramzi Younis. Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case Presentation. Arch Case Rep. 2024: doi: 10.29328/journal.acr.1001099; 8: 075-077
-
Artificial Intelligence in the Pharmaceutical Galenic Field: A Useful Tool with Associated RisksLuisetto M*,Ferraiuolo A,Fiazza C,Cabianca L,Edbey K,Mashori GR,Abdul Hamid G,Latyshev Oleg Yurevich. Artificial Intelligence in the Pharmaceutical Galenic Field: A Useful Tool with Associated Risks. Arch Pharm Pharma Sci. 2025: doi: 10.29328/journal.apps.1001066; 9: 014-020
-
Microcystic Meningioma: Atypical Meningioma Revisited. Rare Case Report with Review of LiteratureKaustubh Gupta*. Microcystic Meningioma: Atypical Meningioma Revisited. Rare Case Report with Review of Literature. J Radiol Oncol. 2025: doi: 10.29328/journal.jro.1001079; 9: 046-049
-
Clinical Severity of Sickle Cell Anaemia in Children in the Gambia: A Cross-Sectional StudyLamin Makalo,Samuel A Adegoke,Stephen J Allen,Bankole P Kuti,Kalipha Kassama,Sheikh Joof,Aboulie Camara,Mamadou Lamin Kijera,Egbuna O Obidike. Clinical Severity of Sickle Cell Anaemia in Children in the Gambia: A Cross-Sectional Study. J Hematol Clin Res. 2025: doi: 10.29328/journal.jhcr.1001033; 9: 001-006
Most Viewed
-
Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth EnhancersH Pérez-Aguilar*, M Lacruz-Asaro, F Arán-Ais. Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth Enhancers. J Plant Sci Phytopathol. 2023 doi: 10.29328/journal.jpsp.1001104; 7: 042-047
-
Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case PresentationJulian A Purrinos*, Ramzi Younis. Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case Presentation. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001099; 8: 075-077
-
Feasibility study of magnetic sensing for detecting single-neuron action potentialsDenis Tonini,Kai Wu,Renata Saha,Jian-Ping Wang*. Feasibility study of magnetic sensing for detecting single-neuron action potentials. Ann Biomed Sci Eng. 2022 doi: 10.29328/journal.abse.1001018; 6: 019-029
-
Pediatric Dysgerminoma: Unveiling a Rare Ovarian TumorFaten Limaiem*, Khalil Saffar, Ahmed Halouani. Pediatric Dysgerminoma: Unveiling a Rare Ovarian Tumor. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001087; 8: 010-013
-
Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative reviewKhashayar Maroufi*. Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative review. J Sports Med Ther. 2021 doi: 10.29328/journal.jsmt.1001051; 6: 001-007

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."